2017 March Report of the Auditor General of Canada Health Care Services—Nunavut
2017 March Report of the Auditor General of Canada Health Care Services—Nunavut
Table of Contents
- Introduction
- Findings, Recommendations, and Responses
- Supporting health centre personnel
- Orientation and training were not consistently delivered to nurses and other selected health centre personnel
- Quality assurance procedures for ensuring and improving the quality of health services were seldom implemented
- Safety risks facing health centre personnel were not adequately managed
- The recruitment of permanent nurses and other health care personnel was ineffective
- Planning and resourcing health centres
- Supporting health centre personnel
- Conclusion
- Subsequent Events
- About the Audit
- List of Recommendations
- Exhibits:
- 1—Air links between Nunavut communities and the locations where residents may be flown if they cannot receive needed health care in their own community
- 2—For selected indicators, the population of Nunavut has a lower health status than the Canadian average
- 3—Quality assurance activities were not conducted as required by Department of Health policy (2014–15 and 2015–16 fiscal years)
Introduction
Background
1. Challenges of delivering health care services. Delivering health care services in Nunavut is challenging for several reasons—size of the territory, dispersion of the small population, weather, and reliance on air transportation. The territory’s 25 communities are isolated and spread across the largest territory or province in Canada.
2. Nunavut’s communities are accessible year round only by air, which plays an important role in delivering health care. Regular commercial flights are used for non-urgent medical travel, while air ambulances are used for medical emergencies. Depending on a patient’s needs and the types and levels of care available in a community, patients may be sent to larger centres for treatment of conditions such as stroke, heart attack, or cancer. These centres include Iqaluit, Rankin Inlet, Cambridge Bay, Yellowknife, Ottawa, Churchill, Winnipeg, and Edmonton (Exhibit 1).
Exhibit 1—Air links between Nunavut communities and the locations where residents may be flown if they cannot receive needed health care in their own community
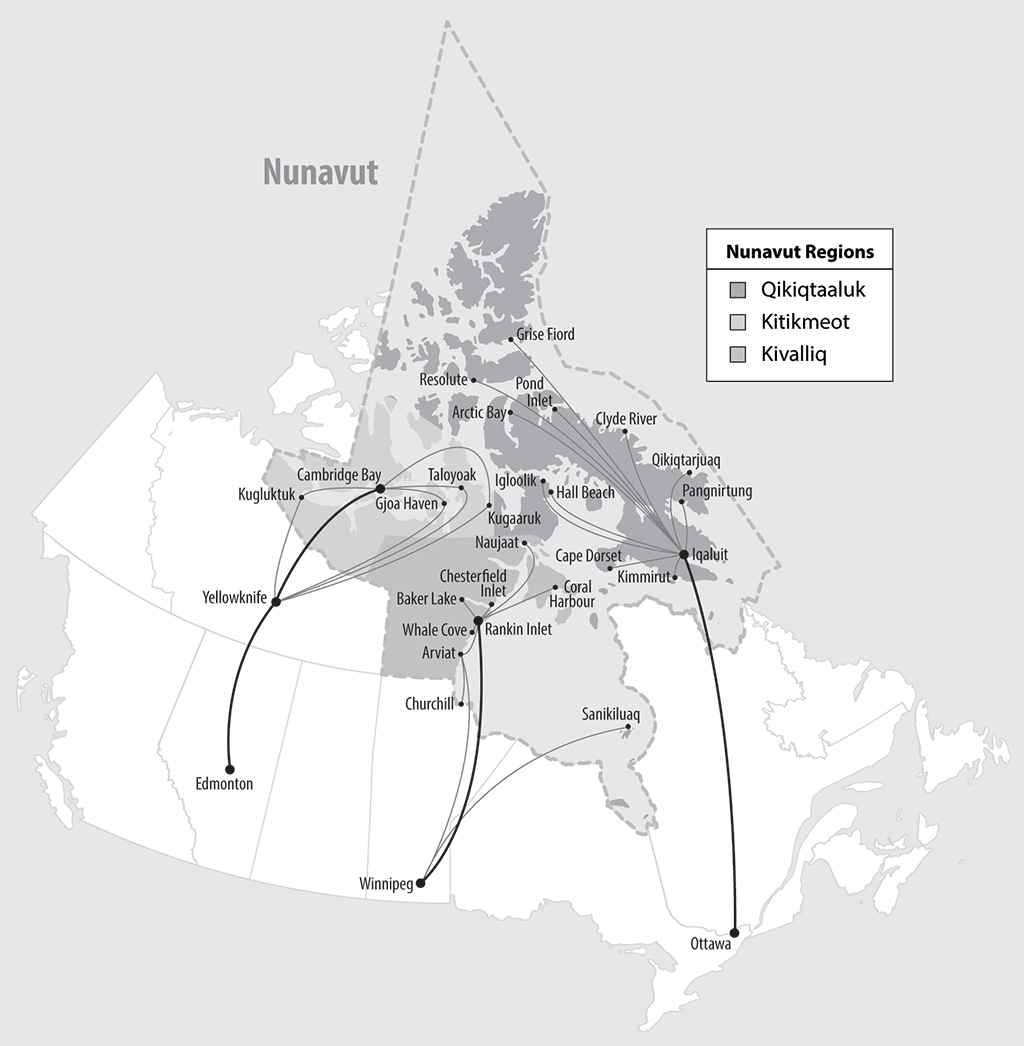
Source: Based on information from the Nunavut Department of Health.
Exhibit 1—text version
The map highlights the three regions in Nunavut—Kitikmeot, Kivalliq, and Qikiqtaaluk—and shows their communities, including their regional centres. Residents may be flown from smaller communities in Nunavut to regional centres or elsewhere in Canada for health services.
| Region (listed alphabetically) |
Nunavut communities (listed alphabetically) |
Regional centres | Larger centres elsewhere in Canada (listed alphabetically) |
|---|---|---|---|
| Kitikmeot | Gjoa Heaven, Kugaaruk, Kugluktuk, Taloyoak | Cambridge Bay | Edmonton, Yellowknife |
| Kivalliq | Arviat, Baker Lake, Chesterfield Inlet, Coral Harbour, Naujaat, Sanikiluaq, Whale Cove | Rankin Inlet | Churchill, Winnipeg |
| Qikiqtaaluk | Artic Bay, Cape Dorset, Clyde River, Grise Fiord, Hall Beach, Igloolik, Kimmirut, Pangnirtung, Pond Inlet, Qikiqtarjuaq, Resolute | Iqaluit | Ottawa |
3. The health care system also serves a population that, for selected indicators, has a lower health status than the Canadian average (Exhibit 2).
Exhibit 2—For selected indicators, the population of Nunavut has a lower health status than the Canadian average
| Health indicator | Nunavut | Canada |
|---|---|---|
| Life expectancy at birth (years) (2007–2009) | 71.6 | 81.1 |
| Infant mortality (per 1,000 live births) (2012) | 21.4 | 4.8 |
| Smoking rate (population aged 12 and over who reported being a current daily smoker) (2013–2014) | 60.6% | 18.7% |
| Respiratory diseases, deaths (such as pneumonia, influenza, and bronchitis) (age-standardized rate of death per 100,000 population) (2005–2007) | 182.9 | 45.0 |
| Suicides and self-inflicted injuries, deaths (age-standardized rate of death per 100,000 population) (2012) | 63.5 | 10.4 |
Source: Health Profile Nunavut: Information to 2014, Department of Health, Nunavut (2016). The numbers have not been audited.
4. Recruiting and retaining health care personnel. Many of Nunavut’s health care personnel—especially nurses and physicians—are from outside the territory. Some nurses are drawn to Nunavut by the increased levels of autonomy and opportunities to perform more medical functions compared with working in southern Canada. Others also come to experience Nunavut’s Inuit culture and way of life.
5. Challenges to recruiting and retaining health care personnel include a high cost of living, expensive travel, and limited job opportunities for spouses. Working in small, isolated communities far from family can also be a disincentive.
6. The Department of Health is responsible for delivering health care services in Nunavut as well as for developing policies and legislation that govern the health care system. According to the Department, Nunavut is the only territory or province where the Department of Health is responsible for directly delivering health care services. The Department needs to work with several other departments to deliver on its roles and responsibilities. Its mission is to promote, protect, and enhance the health and well-being of all Nunavummiut, incorporating Inuit Qaujimajatuqangit (that is, traditional Inuit knowledge and values) at all levels of service delivery and design.
7. The Department’s expenditures in the 2015–16 fiscal year were $419.1 million, with just over $70 million (16.7 percent of total departmental expenditures) spent on medical travel.
8. As of 31 December 2016, the Department of Health had 1,151 permanent positions, of which 615 (53.4 percent) were filled with permanent staff, while 536 (46.6 percent) were vacant. The Department uses temporary staff to fill many of these vacant positions. This includes casually employed nurses (that is, nurses hired on a short-term temporary basis) or nurses contracted from private agencies.
9. Nunavut’s 25 communities receive health services through 22 community health centres, regional health centres in Rankin Inlet and Cambridge Bay, and the Qikiqtani General Hospital in Iqaluit. A public health unit is also located in Iqaluit. The Department of Health also manages long-term care facilities in two communities. The Department expected to become responsible for managing three elder care centres on 1 April 2017.
10. Community health centres are typically staffed by a nurse-in-charge and community health nurses. To work in Nunavut, community health nurses must meet certain minimum education and work experience requirements and be eligible for registration with the Registered Nurses Association of the Northwest Territories and Nunavut.

Community health centre in Pangnirtung, 2016.
Photo: Office of the Auditor General of Canada
11. Physicians and certain specialists periodically visit health centres and provide advice to nurses by phone. The Qikiqtani General Hospital in Iqaluit and the two regional health centres in Cambridge Bay and Rankin Inlet have physicians available full-time. Administrative staff and laboratory technicians located at the Qikiqtani General Hospital and at laboratories in southern Canada also support the work of community health nurses.
12. Community health nurses are the backbone of community health centres. They provide primary assessment, treatment, and consultation. They are also involved in providing pre- and postnatal care, services to patients who have chronic disease(s) such as high blood pressure or diabetes, and immunizations.
13. Community health nurses can also perform an expanded scope of practice that can include tasks such as suturing wounds, dispensing medication, performing certain X-rays, and putting casts on fractured limbs. Working in this expanded scope of practice requires specialized skills, knowledge, and competencies that are beyond traditional nursing education programs. With proper in-service training and education, community health nurses can also perform certain medical functions delegated to them by a physician.
14. Community health centres also have clerk interpreters and caretakers. Clerk interpreters interpret doctors’, nurses’, and other professionals’ questions and explanations for Inuktitut- or Inuinnaqtun-speaking patients while interpreting patients’ replies and questions. Caretakers help with the maintenance and operation of the facility, and perform X-rays.
15. The largest and most equipped health centre in Nunavut is the Qikiqtani General Hospital in Iqaluit. Specialized services such as ultrasounds and laboratory services are provided at regional centres in Rankin Inlet and Cambridge Bay.
Focus of the audit
16. This audit examined whether the Department of Health adequately managed and supported selected health care personnel who deliver services in local and regional health centres in Nunavut. We looked at orientation and training, quality assurance and continuous improvement processes, the management of safety risks facing staff in health centres, and the recruitment of health care personnel. We focused mainly on those involved in providing primary and emergency care: supervisors of health programs, community health nurses, clerk interpreters, and staff responsible for taking X-rays. We also looked at the planning and resourcing of services provided at health centres, particularly in relation to community health nurses and physicians.
17. This audit is important because having the right number and type of staff in health centres, with the training and tools they need to deliver health services, is essential to ensuring that residents of Nunavut receive the health services they need, when and where they need them.
18. More details about the audit objective, scope, approach, and criteria are in About the Audit at the end of this report.
Findings, Recommendations, and Responses
Supporting health centre personnel
Overall message
19. Overall, we found that the Department of Health did not adequately support community health nurses and other selected health care personnel working in community health centres. The Department did not ensure that community health nurses, X-ray takers, and interpreters received the training they needed to work in isolated communities. The Department did not fully implement procedures for assuring the quality of health services and supporting the continuous improvement of its staff and service delivery. It did not adequately manage the safety risks faced by health care personnel in community health centres. We also found that the recruitment of nurses and other selected health care personnel, which is managed by the departments of Health and Finance, was not effective in staffing vacant positions within the Department of Health.
20. These findings are important because providing orientation and ongoing training, assessing and continuously improving the quality of services, providing a safe work environment, and recruiting staff in a timely manner all affect the Department of Health’s ability to deliver services in health centres. How these issues are managed can also affect the Department’s ability to recruit and retain nurses and other health care personnel.
21. As of 31 March 2016, in health centres outside of Iqaluit, there were 69 positions for community health nurses providing primary and emergency care and 25 positions for nurses-in-charge. Of the 69 community health nurse positions, 43 were vacant (62 percent). By region, this rate varied from 60 percent for Qikiqtaaluk (excluding Iqaluit) and Kivalliq to 71 percent for Kitikmeot. In total, 5 of the 25 nurse-in-charge positions were vacant. The Department uses casual and agency nurses to fill these vacancies and to replace permanent nurses on leave.
22. In the 2015–16 fiscal year, Department of Health expenditures on agency nurses were about $16.3 million. Based on information provided by the Department of Finance, the Department of Health spent approximately $15 million on casual nurses in the 2015–16 fiscal year.
23. The Department of Health has authority for the hiring of nurses, midwives, and the management of contracts with physicians and nursing agencies. As part of the staffing process, the Department of Health is also responsible for preparing job descriptions and designing and adjusting the Department’s organizational structure as required. Any organizational changes proposed by the Department must be approved by the Department of Finance and by Cabinet.
24. The Department of Finance is responsible for hiring non-nursing employees, reviewing and evaluating all job descriptions for the Department of Health, and determining the salary of a position. The Department of Finance also develops human resource policies and procedures—such as the requirement for performance appraisals—for the Government of Nunavut.
25. The Department of Health and the Department of Finance work with the Nunavut Housing Corporation to ensure housing units are allocated to eligible employees.
Orientation and training were not consistently delivered to nurses and other selected health centre personnel
26. We found that the Department of Health did not deliver consistent orientation and training to its nurses or selected support staff (X-ray takers and clerk interpreters) working in health centres. The Department did not have annual base funding for orientation and training. Clinical nurse educators, who help manage and coordinate the delivery of orientation and training to nurses, were not all in place. There was also no systematic tracking of the orientation and training received by community health nurses and support staff, including whether their certifications were up to date.
27. Our analysis supporting this finding presents what we examined and discusses
- orientation and training offered to selected health centre personnel, and
- tracking of orientation and training.
28. This finding matters because providing consistent orientation and training helps the Department of Health ensure its personnel—such as community health nurses, X-ray takers, and interpreters—develop and maintain the skills and competencies they need to carry out their duties.
29. Our recommendations in these areas of examination appear at paragraphs 39 and 41.
30. What we examined. We examined whether the Department of Health
- had orientation and training programs in place for community health nurses and selected support staff,
- adequately delivered and managed these programs, and
- had systems in place to track the orientation and training delivered to and received by staff.
31. Orientation and training offered to selected health centre personnel. Orientation is important in assisting new employees to understand the social, technical, and cultural aspects of working in a health centre. Orientation can also inform nurses of the Department of Health’s policies on when and how they can perform advanced nursing functions and medical functions delegated by a physician.
32. Training helps nurses develop and maintain the skills and competencies necessary to carry out their duties and maintain their registration with the Registered Nurses Association of the Northwest Territories and Nunavut. It is also important for helping nurses maintain certifications, such as those for cardiopulmonary resuscitation (CPR) and immunization. Without adequate training and competencies, nurses cannot perform advanced nursing and delegated medical functions.
33. We found that the Department of Health provided orientation and training to its nurses on an inconsistent basis, and that training varied across regions in terms of scope and accessibility. The type of orientation and training offered depended in part on the availability and experience of the staff in place. Department officials told us that some community health nurses had not received adequate orientation and training to perform delegated medical functions; therefore, they were not prepared for their roles in the communities.
34. The Department of Health had three clinical nurse educator positions to help develop, coordinate, and deliver orientation and training to nurses. The positions were in the Kivalliq and Qikiqtaaluk regions and the Qikiqtani General Hospital in Iqaluit. We found that the position in Iqaluit had been filled since 2013. The position in the Qikiqtaaluk region became vacant in January 2016 and was being filled on a temporary basis. The position for the Kivalliq region was filled, but the person was acting in another position. The Kitikmeot region did not have a clinical nurse educator position.
35. We also examined the training provided to health centre support staff, such as caretakers and clerks, who perform X-rays. X-rays are an important diagnostic tool for chronic and acute conditions, such as tuberculosis, or specific injuries like broken bones.
36. Several Department officials told us that there was a lack of training for X-ray takers. In addition, a review completed in June 2015 for the Department found significant concerns with the lack of skills and training available to staff performing X-rays. One of the analyses concluded that 45 percent of the 711 X-ray images taken in certain community health centres in the 2014–15 fiscal year were of poor quality for diagnostic purposes, raising concerns about risks to patients, staff, and the Department. Although some training sessions were offered since then, we found that most of the X-ray takers we met had not taken training, felt more was needed, or had not taken training in many years.
37. We also examined what training was offered to clerk interpreters to provide interpretation services in a medical environment. We found that there was a non-mandatory course on medical terminology available in Iqaluit, Rankin Inlet, and Cambridge Bay for clerk interpreters. We found that several clerk interpreters we met had not received such training, had not received it in a timely manner, or had not taken training in many years. Having interpreters with knowledge of medical terminology and vocabulary is important because it helps Inuit patients who do not speak English and their health care providers better understand each other about, for example, the patient’s conditions.
38. We found that the Department of Health did not have annual base funding for orientation and training. According to the Department, training was funded through external grants or internal non-training budgets, making it difficult to plan and deliver necessary training.
39. Recommendation. The Department of Health should ensure that appropriate orientation and training are made available on a timely basis to its health care personnel.
The Department of Health’s response. Agreed. The Department of Health will formalize a plan to provide structured clinical orientation and training to health care personnel and will collaborate with the Department of Culture and Heritage on cultural orientation to ensure that it is provided in a timely manner to all new employees.
40. Tracking of orientation and training. Systematic tracking of orientation and training would let the Department of Health know whether nurses and other health care personnel have adequate and up-to-date skills and competencies. It would also help identify needs. We found that the Department of Health did not systematically track orientation or training taken by community health nurses and support staff. There was also no systematic monitoring of the licences and certifications requiring renewal (such as cardiopulmonary resuscitation and immunization) after a community health nurse was hired.
41. Recommendation. The Department of Health should put in place systems to track and monitor whether its health care personnel have taken orientation and training in a timely manner and if licences and certifications are up to date.
The Department of Health’s response. Agreed. The Department of Health will formalize and implement a plan to track and monitor training, orientation, licensing, and certifications on an ongoing basis.
Quality assurance procedures for ensuring and improving the quality of health services were seldom implemented
42. We found that the Department of Health had procedures to assess and continuously improve the quality of care offered by staff in community health centres. However, the procedures were seldom implemented and the Community Health Nursing Administration Manual was not up to date. Monthly audits of selected patient charts, annual reviews of these audits, annual visits to community health centres by directors of health programs, performance appraisals of nurses, and the reporting and tracking of incidents related to patient care were not conducted as required.
43. Our analysis supporting this finding presents what we examined and discusses
- quality assurance procedures;
- reporting, tracking, and analyzing incidents related to patient care; and
- the Community Health Nursing Administration Manual.
44. This finding matters because up-to-date and fully implemented procedures to assess and continuously improve the quality of care being offered by staff in community health centres helps the Department of Health ensure the quality of care. It would also inform its nurses on current best medical procedures and help to identify and address practices that are not in line with Departmental policies. The lack of quality assurance can lead to medical errors occurring, putting patient health at risk.
45. Our recommendations in these areas of examination appear at paragraphs 55, 58, and 61.
46. What we examined. We examined whether the Department of Health followed its procedures to assess and continuously improve the quality of care being offered through community health centres.
47. Quality assurance procedures. The Department of Health requires staff to conduct several quality assurance procedures, which include monthly audits of patient charts, annual reviews of these audits and annual visits to community health centres by regional directors of health programs, performance appraisals, and incident reporting. We found that these procedures were seldom implemented.
48. The Department of Health requires nurses-in-charge at health centres (the supervisors of health programs) to conduct monthly audits of eight patient charts filled out by community health nurses. Chart audits must be submitted monthly to the Director of Health Programs in each region.
49. Such audits are considered essential quality assurance activities, and are an opportunity for nurses-in-charge to teach and to enhance nursing practices. Patient charts are important for documenting the results of patient visits to a health centre. Charts include a description of the individual’s health condition, diagnosis, proposed care plan, and referrals (if appropriate). Well-documented patient charts promote consistency and continuity of patient care.
50. We found that the required monthly audits of patient charts were seldom done. We requested monthly chart audits received by the Director of Health Programs in each region for our two-year audit period for the seven communities we visited. We received 259 (19.3 percent) of the 1,344 chart audits that were supposed to have been completed (Exhibit 3).
51. Each year, a review is to be conducted by the Director of Health Programs of all completed chart audits in their region. These reviews are intended to identify nursing trends and factors that influence the quality of nursing care and to help continuously improve nursing practices. We found that these yearly reviews of chart audits were not completed.
52. The Department of Health also requires that the Director of Health Programs in each region visit each community health centre at least once per year. These visits help ensure that action is taken to eliminate potential or actual problems and concerns in health centres regarding such topics as the delivery of health programs, workplace health and safety, and workload. During our two-year audit period, 2 annual visits to community health centres were required for each of the seven communities we visited (14 in total); we found that only 2 of the 14 were completed as required (Exhibit 3).
53. We also examined nursing performance appraisals. The Government of Nunavut Human Resources Manual requires that annual performance appraisals be conducted for all permanent employees to support continual improvement. We looked at the performance appraisals completed for nurses in the seven communities we visited. We found that 43.9 percent of performance appraisals of permanent nurses were completed (Exhibit 3).
Exhibit 3—Quality assurance activities were not conducted as required by Department of Health policy (2014–15 and 2015–16 fiscal years)
| Quality assurance activity | Number required (based on 7 communities visited) | Number provided to audit team |
|---|---|---|
| Monthly chart audits (8 charts per community health centre per month) | 1,344 | 259 (19.3% of required chart audits) |
| Annual community health centre visits (1 per year) | 14 | 2 (14.3%) |
| Performance appraisals for permanent nurses | 41 | 18 (43.9%) |
Source: Based on information provided by the Department of Health. The numbers have not been audited.
54. According to the Human Resources Manual, there were no specific requirements to complete performance appraisals for casual and agency nurses. Nursing agencies are expected to provide qualified nurses with appropriate orientation and training. Nonetheless, it is our view that conducting and tracking appraisals for casual and agency nurses could be useful for identifying these nurses’ training needs and their strengths and weaknesses, and for informing future hiring and contracting decisions.
55. Recommendation. The Department of Health should, in collaboration with the Department of Finance, develop and implement procedures for assessing and tracking the performance of casual and agency nurses.
The Department of Health’s response. Agreed. The Department of Health will engage in discussion with the Department of Finance on the amendment of the process to develop the necessary forms to accurately assess performance of casual health care staff and to secure a method to track and report on the performance of casual employees.
The Department of Finance’s response. Agreed. The Department of Finance will work with the Department of Health to address performance reviews for casual and agency nurses, where appropriate, for the purpose of rehiring individuals.
56. Reporting, tracking, and analyzing incidents related to patient care. Department of Health guidelines require that a tracking system be developed and maintained to document risks to the Department, including incidents related to patient care.
57. We found that the Department of Health did not track the number or type of incidents involving patient care. As a result, the Department could not adequately analyze such incidents to identify problems and trends, address root causes, and effectively manage risks related to patient safety and quality of care. We asked for incident reports related to patient care and received a total of 93 from different sources for our two-year audit period. We were told that these were only a portion of the incident reports produced, and that incidents were underreported. Examples of issues in incident reports we received included dispensing inappropriate medications, providing wrong vaccine doses, and delaying the provision of care. The Department of Health began developing new policies for incident reporting; however, at the time of our audit, these had not been finalized.
58. Recommendation. The Department of Health should ensure that its procedures for assuring and continuously improving the quality of its health care services are implemented according to departmental policy, including those related to monthly audits of patient charts and related annual reviews, annual visits to community health centres, performance appraisals, and incident reporting. It should also put systems in place to ensure that the findings resulting from these procedures are followed up on and implemented.
The Department of Health’s response. Agreed. The Department of Health will formalize a plan for the implementation of quality assurance that will include all aspects of the Office of the Auditor General of Canada’s recommendations.
59. The Community Health Nursing Administration Manual. We examined whether the Department of Health kept its Community Health Nursing Administration Manual up to date. The policies in the manual are intended, among other things, to promote consistent nursing care throughout the territory and reduce clinical errors and incidents. The manual also identifies which medical functions performed by registered nurses require additional training or consultation with a physician beforehand.
60. The manual requires that the Department of Health develop, review, and revise the manual’s nursing policies and guidelines as legislation, best practices, and policies change. We found that this had not been done since 2011. Department officials expressed concerns to us that some of the manual’s policies were out of date and did not reflect current best practices. Ensuring that staff are aware of changes to departmental policies is important. We noted that in early 2016, the Department began sending a newsletter from the Deputy Minister to all staff that communicated, among other things, clinical policy updates.
61. Recommendation. The Department of Health should ensure that its nursing manual is kept up to date and is well communicated to staff in health centres.
The Department of Health’s response. Agreed. The Department of Health will develop a schedule and procedure for the ongoing review and revision of the nursing manual.
Safety risks facing health centre personnel were not adequately managed
62. We found that the Department of Health did not adequately manage the safety risks to its health centre personnel. The Department did not assess risks to work site safety in community health centres and did not track safety-related incidents. In addition, we found that occupational health and safety committees were non-existent or not active in most health centres. Security measures, such as panic alarm systems, were not always operational or adequate for staff security.
63. Our analysis supporting this finding presents what we examined and discusses
- assessing safety risks and tracking safety-related incidents,
- safety guidelines,
- occupational health and safety committees, and
- security measures.
64. This finding matters because the Department of Health is required by the Safety Act and Government of Nunavut policies to provide a safe work environment for health centre personnel. An unsafe work site could result in harm to employees. It can also create liabilities for and affect the reputation of the Department of Health and the Government of Nunavut. Providing for a safe work environment can help the Department of Health reduce these risks. Not adequately managing risks in the work site can also affect the recruitment and retention of health centre personnel.
65. Our recommendations in these areas of examination appear at paragraphs 70 and 79.
66. What we examined. We examined whether the Department of Health provided a safe environment for health centre personnel. In particular, we examined whether the Department
- assessed the safety risks in the community health centres,
- tracked safety-related incidents and took appropriate mitigation actions,
- had appropriate selected safety guidelines for employees,
- ensured that occupational health and safety committees were in place in health centres, and
- implemented adequate security measures in health centres.
67. Assessing safety risks and tracking safety-related incidents. It is a best practice in the occupational health and safety field to conduct a work site risk assessment to identify situations that may cause harm to people. This includes health centres, where there may be risks to the safety of staff. We were told that the Department of Health did not conduct risk assessments of the safety of the community health centres. Consequently, it did not have a complete picture of the risks faced by its staff working in health centres. This limited its ability to identify and implement appropriate safety measures.
68. We also found that there was no clear direction on incident reporting related to staff safety, and no central repository or tracking within the Department of Health for these incident reports. We received evidence from different sources at the Department of 41 safety-related incidents that occurred in health centres across the territory during the 2014–15 and 2015–16 fiscal years. The safety-related incidents included staff receiving verbal and physical abuse, threats from patients, and break-ins at health centres. In 2015, the Department of Finance and the Department of Health agreed that incident reports would be sent to the Department of Finance’s risk management team. This was an interim arrangement until the Department of Health implemented its own tracking system. The Department of Finance provided us with information on 8 additional safety-related incidents involving health centres.
69. Because the Department of Health did not track safety-related incidents, it did not have a complete picture of the number and nature of safety incidents that had occurred. In our view, the Department of Health should have complete information on the number and nature of safety-related incidents in health centres so that it can assess risks and take appropriate actions.
70. Recommendation. The Department of Health should systematically track and monitor safety-related incidents and take appropriate follow-up actions to correct or mitigate safety-related risks.
The Department of Health’s response. Agreed. The Department of Health will develop a health and safety strategy to include the tracking and statistical analysis of all health and safety-related incidents to ensure the proper actioning and allocation of resources to reduce risks.
71. Safety guidelines. The Department of Health did identify that staff working alone (such as at night or on weekends) was a risk. Nurses in Nunavut may have to go alone to the health centre after working hours or during winter weather conditions to respond to an emergency. People working alone might not be able to get immediate assistance in the event of injury, ill health, or emergency. To mitigate this risk, the Department of Health created safety guidelines in 2014 for when health centre staff are working alone, along with other safety guidelines.
72. Several Department officials considered that the Department’s guidelines for staff working alone were not realistic for community health centres. For example, the guidelines indicated that the nurse on call should inform the second or third nurse on call when seeing patients outside of working hours, and update them upon leaving the community health centre. According to the guidelines, the nurse should be accompanied by another nurse if the situation is considered volatile. However, Department officials indicated that these guidelines were not appropriate and were difficult to apply. For example, it can be difficult to predict if a patient will become violent or aggressive. Moreover, if the first nurse on call has to go to the health centre several times during the night, the second nurse on call would be disturbed, which could have an impact on services delivered the next day.
73. According to a survey of community health nurses working outside of Iqaluit conducted by the Department of Health in 2015, many respondents said that they were worried about their safety while on call.
74. Occupational health and safety committees. At the time of our audit, territorial legislation required that work sites with more than 10 employees have an occupational health and safety committee. The responsibilities of these committees include identifying the risks involved and making recommendations to reduce or eliminate them. We found that most of the health centres with more than 10 employees did not have an active health and safety committee in place, affecting the Department’s ability to assess, identify, and manage safety risks.
75. We noted that in 2014, the Department of Health requested funding to create an occupational health and safety program. However, except for funding for a territorial infection prevention and control practitioner, the funding was denied because the Department of Finance already had an occupational health and safety team in place that serves the whole Government of Nunavut.
76. Security measures. According to the Safety Act, the Department of Health is required to take all reasonable precautions and adopt and carry out all reasonable techniques and procedures to ensure the health and safety of every person in its work site. The Department had implemented some security measures at all health centres (such as panic and intrusion alarms). However, the Department recognized that these measures were not uniformly implemented and were largely ineffective or not functioning.
77. The Pangnirtung health centre was the only health centre with security guards. According to the Department, the presence of security guards helped to improve safety at that health centre. Guards were brought in following safety incidents, such as break-ins, at the centre.
78. The Department has to comply with new occupational health and safety requirements as a result of legislative changes in March 2016. These include new rules for establishing occupational health and safety committees, implementing effective communication systems, and developing and implementing a written policy to deal with potential violence. Given the risks faced by the community health centres, it will be important to implement these measures rapidly.
79. Recommendation. The Department of Health should, in collaboration with other departments, provide a safe and secure work environment for its health care personnel by implementing adequate procedures such as risk assessments and appropriate security measures. The Department should ensure that the security measures it implements are monitored, known, and working properly.
The Department of Health’s response. Agreed. The Department of Health will collaborate with the Department of Community and Government Services and the Department of Finance (Risk Management) to ensure that risks are identified and analyzed and that proper action is taken to address and reduce the potential for accident and injury.
The recruitment of permanent nurses and other health care personnel was ineffective
80. We found that the recruitment of permanent nurses and other health care personnel was ineffective. There were significant delays in staffing actions, which were caused by many factors. The Department of Health did not have documented procedures, service standards, or an effective system for tracking and managing its staffing actions. We found that the terms and conditions of employment offered to permanent, casual, and agency nurses were not assessed to determine if they were competitive with those offered in other jurisdictions. The Department of Health had limited capacity in its human resource function, especially given the workload it faced. The lack of housing and sufficient space in health centres also contributed to staffing delays. In addition to the recruitment delays, the Department of Health did not have an up-to-date recruitment and retention strategy for nurses.
81. Our analysis supporting this finding presents what we examined and discusses
- timely recruitment,
- assessing terms and conditions of employment,
- human resource capacity,
- housing and office space, and
- recruitment and retention strategy for nurses.
82. This finding matters because timely and effective recruitment and staffing could help the Department of Health develop a stable, qualified workforce. It can also reduce the Department’s dependency on casual and agency nurses, which can affect the continuity of care provided to patients and increase the workload of permanent staff.
83. Our recommendations in these areas of examination appear at paragraphs 91, 92, 97, 98, 100, and 103.
84. What we examined. We examined whether the Department of Health, in coordination with the Department of Finance, managed recruitment and staffing in a way that met its staffing needs. We interviewed officials from both departments and reviewed the staffing actions for 72 clinical and non-clinical positions across the three regions. This included staffing actions related to supervisors of health programs (the nurses in charge of health centres), community health nurses, nurse practitioners, radiologists, ultrasonographers, clerk interpreters, and selected senior management positions.
85. Timely recruitment. We found that the staffing process was lengthy. As a result, many of the permanent positions we examined were vacant for a long time—in some cases, for many years. The lengthy vacancies for permanent positions was one reason why the Department of Health relied heavily on temporary staff. The high use of temporary staff can affect the continuity and quality of care provided to patients. Using a high number of temporary staff to fill nursing vacancies can also place extra pressure on permanent community health nurses and supervisors of health programs, who have to train and orient new staff to the health centre—taking time away from their existing duties and leading to higher workloads or other tasks not getting done.
86. We found that various internal and external factors lengthened the staffing process. For example, we found instances where
- the Department of Health did not take timely actions to start a staffing process after a position became vacant,
- the Department of Health submitted to the Department of Finance incomplete and/or inaccurate information regarding staffing actions,
- there was a lack of timely communication between the two departments,
- there was a lack of suitable candidates for a position, and
- successful candidates had declined job offers.
87. Based on information the Department of Health and the Department of Finance provided, we found that the Department of Health took an average of 222 calendar days to start a staffing action after a position became vacant. It also took an average of 160 calendar days to advertise the position after the start of the staffing action. This included an average of 21 calendar days to process the staffing request at the Department of Finance, which conducts a job evaluation before any position is advertised. This included time taken by the Department of Finance to collect additional information, when necessary, from the Department of Health to complete the evaluation. For the majority of cases (69 percent), the job evaluation process took fewer than 20 calendar days. For the 25 staffing actions that were successfully completed during our audit period, it took an average of 562 calendar days (or about 18 months) to hire a new employee after a position became vacant.
88. We examined the tracking of staffing actions and the departments’ service standards regarding the timeliness of staffing actions. Documented procedures, along with appropriate support and guidance, are important for informing staff of what information is required when submitting staffing requests and for preventing incomplete or inaccurate requests from being submitted. Service standards are important for setting expectations regarding how long staffing actions should take under normal circumstances.
89. While the Department of Health must follow the general staffing procedures established for all territorial departments, we found that the Department did not have documented procedures or service standards for its own recruitment and staffing activities. In addition, we found that the Department of Health did not have an effective means of tracking and recording the information related to staffing actions, making it difficult to track the status of the staffing actions, identify reasons for delays, and take appropriate corrective actions. We noted that in March 2015, the Department of Health submitted a request to purchase a human resource recruitment software that would help it process job applicants from posting to hiring. At the end of our audit period, the request had not been processed by the Department of Community and Government Services.
90. We found that unlike the Department of Health, the Department of Finance had put in place written procedures and service standards regarding its recruitment and staffing activities. This included a five-business-day service standard for completing job evaluations, once complete information had been received by the department doing the hiring. The Department of Finance also had systems for tracking and reporting on the status of staffing actions. However, we noted that the Department of Health did not receive status reports on staffing actions managed by the Department of Finance. Also, the Department of Finance did not assess its performance against its service standards. The Department of Health indicated that it would be useful to have access to the Department of Finance’s staffing action information to keep up to date and to improve collaboration between the two departments.
91. Recommendation. The Department of Health should develop procedures and service standards for its recruitment and staffing actions. The Department, with the collaboration of the Department of Finance and other relevant departments, should put systems and practices in place to track and record information related to vacancies and associated staffing actions, and look for opportunities to streamline the hiring process.
The Department of Health’s response. Agreed. The Department of Health will collaborate with the Department of Finance to improve information sharing and streamline the staffing process. The Department of Health will also develop standards and procedures to improve efficiency and expedite the hiring process.
The Department of Finance’s response. Agreed. The Department of Finance will work on improving its internal information systems and on sharing this information with the Department of Health and other departments.
92. Recommendation. The Department of Health and the Department of Finance should monitor the status of staffing actions and take appropriate action to reduce delays. This should include monitoring against their service standards.
The Department of Health’s response. Agreed. The Department of Health will collaborate with the Department of Finance to improve information sharing to reduce delays and monitor performance against service standards.
The Department of Finance’s response. Agreed. The Department of Finance will collaborate with the Department of Health to improve information sharing to reduce delays and monitor performance against service standards.
93. Assessing terms and conditions of employment. An important step when filling a position is assigning a salary and other terms and conditions of employment based on an analysis of the position’s roles and responsibilities and of similar positions within the Government of Nunavut. Analysis of similar positions within other provinces and territories could also be used to determine if the conditions of employment are competitive enough to attract qualified candidates.
94. We noted that the Department of Finance conducted market analysis for some specialized health personnel positions when determining salary ranges for the staffing requests it received from the Department of Health. However, for certain specialized positions, the Department of Health felt that the Department of Finance assigned a salary that was not competitive—for example, with other markets—and would be a barrier to finding qualified permanent staff.
95. Through interviews with nurses and other officials in the Department of Health, and a documentation review, we found that the terms and conditions of employment offered to permanent nurses, such as compensation, accommodation allowance, and work schedule, were not considered attractive by the nurses compared with conditions offered to agency or casual nurses. Department officials stated that some of the conditions hurting its ability to recruit permanent nurses were the lack of flexibility and opportunities to take time off and travel out of the territory. This was considered important given the high level of stress experienced in community health centres.
96. The Department of Health and the Department of Finance recognized the discrepancies in the terms and conditions between permanent and casual nurses, and had taken action to adjust the terms and conditions for casual nurses. However, we found that neither department had done any benchmarking analysis with other jurisdictions.
97. Recommendation. The Department of Finance and the Department of Health should work together to ensure that the terms and conditions of employment for health care positions are competitive, and should analyze the terms and conditions of employment in other provinces and territories when applicable.
The Department of Finance’s response. Agreed. The Department of Finance will collaborate with the Department of Health to develop market analysis and methodology for addressing any identified gaps in compensation for health care personnel to ensure that Nunavut is viewed by health care personnel as an employer of choice.
The Department of Health’s response. Agreed. The Department of Health will seek assistance from the Department of Finance to develop market analysis and methodology for addressing gaps in compensation for health care personnel to ensure that Nunavut is viewed by health care personnel as an employer of choice.
98. Recommendation. The Department of Health, in collaboration with the Department of Finance, should assess the market conditions for permanent, agency, and casual nurses; compare the results with other jurisdictions; and take appropriate actions based on this analysis to increase the competitiveness of these positions and facilitate the hiring of permanent nurses.
The Department of Health’s response. Agreed. The Department of Health will seek assistance from the Department of Finance to conduct a jurisdictional scan on compensation and non-monetary benefits across employment types to ensure that permanent employment is viewed as the most attractive employment option.
The Department of Finance’s response. Agreed. The Department of Finance will collaborate with the Department of Health to conduct a jurisdictional scan on compensation and non-monetary benefits across employment types to ensure that permanent employment is viewed as the most attractive employment option.
99. Human resource capacity. Officials from the Department of Health raised concerns regarding the lack of capacity within its human resource function to manage its recruitment and staffing demands. This included lack of appropriate skills and experience in human resource management. We found the Department of Health was centralizing its staffing and recruitment functions, moving responsibilities from regional offices to its headquarters in Iqaluit, in an effort to streamline the staffing process. Furthermore, the Department was planning to use a specialized recruitment firm to recruit nurses on its behalf.
100. Recommendation. The Department of Health should complete the implementation of the recent initiatives to improve its human resource function, periodically assess the efficiency of these initiatives, and take appropriate actions on the results of these assessments.
The Department of Health’s response. Agreed. The Department of Health continues to work toward meeting deliverables outlined in the Department’s human resource strategy. Once completed, the strategy, which ends in 2017, will be evaluated and new actions will be included in the 2017–2020 strategy.
101. Housing and office space. Officials from the Department of Health informed us that the lack of housing and office space within health centres was a barrier to hiring nurses and health care personnel. In seven of the staffing actions for the 72 positions we examined, lack of housing or office space was a factor that delayed the hiring process. According to the Department of Health, some of the space it required was not available due to the fact that the Department of Family Services retained space within selected health centres after that department was created in 2013.
102. Recruitment and retention strategy for nurses. The Department of Health produced a nursing recruitment and retention strategy for 2007 to 2012. The Nunavut Nursing Recruitment and Retention Strategy was designed to reduce the Government of Nunavut’s nursing vacancy rate from its historical range of 30 to 40 percent to a range of 15 to 20 percent by 2012. Although the Department continued to have challenges recruiting community health nurses, there has been no update to the strategy since 2012.
103. Recommendation. The Department of Health should develop and implement an up-to-date nursing recruitment and retention strategy.
The Department of Health’s response. Agreed. The Department of Health has begun work on the new Health Professionals Recruitment and Retention Strategy, which includes nurses and other key health care staff. Non-monetary items will be implemented immediately, and monetary items will be prepared for discussion during the next contract negotiations, which will take place after the expiry of the current collective agreement in 2018.
Planning and resourcing health centres
The Department of Health did not adequately plan the staffing of health centres
Overall message
104. Overall, we found that the Department of Health did not adequately plan the staffing of health centres. It did not adequately account for the changing health care needs of Nunavummiut. As a result, the Department did not have assurance that its health centres had the right number and mix of staff to meet demands. Though the Department recently started to look at how it delivers health care services, it did not expect to consult with Nunavummiut until it had identified options related to how it delivers health care.
105. This finding matters because properly staffing health centres would help ensure nurses and other personnel have a balanced workload, minimizing the need for overtime while contributing to providing quality services. It could also help improve the Department’s ability to recruit and retain health care personnel. Consulting Nunavummiut on the design and delivery of health care services would help the Department take into account Nunavummiut needs and priorities.
106. Our analysis supporting this finding presents what we examined and discusses
- defining types and levels of services,
- human resource planning for the Department of Health,
- quality of information on the health of Nunavummiut for planning and decision making, and
- consulting with Nunavummiut on improving service delivery.
107. According to the Nunavut Bureau of Statistics, as of 1 July 2016, Nunavut had an estimated population of 37,082. Iqaluit, the capital, had a population of 7,590. Nunavut’s remaining communities ranged from fewer than 500 residents to about 2,800. According to the Government of Nunavut, Nunavut’s population increased by 31.8 percent between 2001 and 2016. The Government of Nunavut expects that the population will approach 43,000 in 2025 (an increase of about 52 percent from 2001).
108. In addition to having one of the fastest-growing populations in Canada, Nunavut also has a young population. As of 1 July 2016, 30.1 percent of the population was below the age of 15, compared with 16.1 percent on average in Canada. Meanwhile, since 2001, the number of persons 65 years of age and over had more than doubled in the territory, going from 618 in 2001 to 1,469 in 2016.
109. In addition to population changes, the health care needs and the expectations of Nunavummiut have also changed, and new technologies, such as telehealth, have provided opportunities to enhance the delivery of health care services.
110. Our recommendations in these areas of examination appear at paragraphs 118, 120, 122, and 125.
111. What we examined. We examined whether the Department of Health had defined the types and levels of health services required to address the needs of Nunavummiut and whether a human resource plan was in place to help ensure the right type of resources were in place to address these needs. We also examined whether key decision makers had access to appropriate data to inform resourcing of health services delivered in community health centres. Finally, we examined whether the Department consulted Nunavummiut on the design and delivery of health care services.
Nurse practitioners—Registered nurses who have additional education and nursing experience and who assume broader roles and responsibilities, such as diagnosing and treating illnesses, ordering and interpreting medical tests, and prescribing medication.
112. Defining types and levels of services. We found that the Department of Health had conducted initiatives and analyses on the types and levels of services provided by particular health care personnel in Nunavut, such as nurse practitioners, midwives, and pediatricians. However, we did not find similar analyses for community health nurses and physicians.
113. Department officials told us that the size of communities had increased and demands for health care services had become more complex due to factors such as an increase in the incidence of chronic diseases. While nurse practitioner positions have been created in several communities, no significant changes have been made to the number of community health nurses working in communities. Concerns were raised about the high workload facing these nurses in some of the communities we visited and the impact this could have on the quality of care.
114. The Department was also not able to provide us with historical data on the ratio of community nurses to community populations or how the number of nurses in individual communities had changed over time. This type of information would be useful to determine if and what adjustments should be made to ensure that health care centres are properly staffed to meet demands.
115. Regarding physicians, we found that the Department did not have a formal policy or formula for determining the number of physicians needed per community or the frequency and length of physician visits. The Department was not aware of any needs assessment done for family physicians in Nunavut. As a result, the Department of Health did not have assurance that the number of physicians and the frequency and length of community visits were adequate. Although the Department of Health did not assess the needs for physician services, it has been successful in increasing the number of days that physicians provided services in Nunavut.
116. We were told that the Department’s “rule of thumb” for scheduling physician visits is 5 days of service per 28 days for a population of 1,000. We found that the Department did not meet this informal guideline for four of the five communities we visited that did not have physicians available full-time.
117. In 2015, the Department of Health began to develop and implement a new service delivery model based on best practices for rural and remote communities. The redesign was expected to identify the current health care services needed, potential new ways to deliver the services to meet the needs, the type and level of required personnel, and opportunities for new technologies, like telemedicine and mobile ultrasound.
118. Recommendation. The Department of Health should continue its efforts to review and improve how it delivers services to Nunavummiut. The Department should also put in place procedures that allow it to periodically assess how it delivers services to ensure that health centres are able to meet the demographic changes and needs of communities.
The Department of Health’s response. Agreed. The Department of Health is currently working on a new model. Once implemented, the model will be assessed and follow-up consultations will be held per article 32 of the Nunavut Land Claims Agreement.
119. Human resource planning for the Department of Health. A human resource plan is important to ensure that resources are allocated based on the types and levels of services needed by Nunavummiut. We found that a three-year Human Resources Strategic Plan (2014–2017) was prepared for the Department of Health in 2014. It included actions and initiatives aimed at strengthening the Department’s human resource management and accountability. However, the plan did not explain how the Department would ensure that health centres are properly staffed and that it has the right number and types of professionals to deliver health care services in Nunavut.
120. Recommendation. The Department of Health should develop and implement a human resource plan that ensures the Department has the right number and types of health care personnel needed to deliver health care services in Nunavut.
The Department of Health’s response. Agreed. A personnel mix strategy is included in the model of care project that is currently under way. This project is currently assessing health care centre needs and the personnel required to deliver those services and is expected to be completed by 31 March 2017.
121. Quality of information on the health of Nunavummiut for planning and decision making. Having reliable information on the health status of Nunavummiut and their use of the health care system is fundamental to informing decisions on the types and levels of services to be provided by the Department of Health. Department officials told us that there were issues with the completeness and accuracy of the data being collected, including how many patients visit health centres and why, and the services they receive. Officials told us that this has affected their ability to make sound decisions on the types and levels of services the Department provides.
122. Recommendation. The Department of Health should implement systems and practices to collect and analyze key and meaningful information on the health of Nunavummiut and the services they receive at health centres in order to better inform its planning and decision making on providing health services.
The Department of Health’s response. Agreed. The model of care project will address data collection and analysis requirements identified in the audit. The project is expected to be completed by 31 March 2017.
123. Consulting with Nunavummiut on improving service delivery. The territorial government has a legal obligation to consult with Nunavummiut. According to article 32 of the Nunavut Land Claims Agreement, the Department of Health must involve Nunavummiut in the design and delivery of social and cultural programs. This is important for a number of reasons. It gives the Department an opportunity to understand the needs of communities, gauge satisfaction with current services, and seek input on alternative approaches to how services are delivered. Consultations with Nunavummiut can also help the Department ensure the planned service delivery model mentioned in paragraph 117 takes into account their needs and priorities. We examined the level of consultation with Nunavummiut expected as part of the initiative to develop and implement a new service delivery model for the territory.
124. Department officials told us they expected to consult with Nunavummiut once the Department had identified service delivery options. In our opinion, engaging Nunavummiut at the start of the process, when identifying options on how the current service delivery model can be improved, would provide for a more inclusive process. While research is needed to identify options, early engagement with Nunavummiut is important to the success of the review and the implementation of any changes in how health services are delivered in Nunavut.
125. Recommendation. The Department of Health should ensure that Nunavummiut are involved throughout its current and future reviews of how it delivers health services and programs.
The Department of Health’s response. Agreed. The Department of Health will ensure that all strategy development requirements will continue to meet obligations under article 32 of the Nunavut Land Claims Agreement.
Conclusion
126. We concluded that the Department of Health did not adequately manage and support its health care personnel to deliver services in local and regional health centres in Nunavut. It also did not adequately consider the changing needs of communities when planning the staffing of health centres. In addition, the recruitment of nurses and other health care personnel, which involves both the Department of Health and the Department of Finance, was not effective for staffing vacant positions or meeting the staffing needs of the Department of Health.
Subsequent Events
127. In the 2016–17 fiscal year, the Department of Health continued or began introducing a number of initiatives aimed at strengthening the support it provides to its health care personnel. It also began a review of how it delivers health care services. It is our view that implementation of these initiatives will address some of our audit findings.
128. Orientation and training. For the 2016–17 fiscal year, the Department received about $1.6 million for training (out of $5.65 million it originally requested). It planned to use this funding to set up a standardized training program that would, among other things, develop nurses’ competencies. We noted that about $950,000 of the $1.6 million the Department received was earmarked for enhanced training for staff performing X-rays.
129. In July 2016, a clinical nurse educator position was created for the Kitikmeot Region. Meanwhile, the position in the Qikiqtaaluk region had become vacant. Efforts were under way to staff vacant nurse educator positions.
130. Continuous Quality Improvement Program. The Department of Health received approval for the implementation of a new Continuous Quality Improvement Program starting in the 2016–17 fiscal year. The program’s goal is to improve quality management by examining and improving health care processes, maintaining standards, and promoting best practices. One of the objectives is to lead and evaluate quality improvement initiatives to deliver a more efficient, patient-centred health care system.
131. Intranet site for policies. In the 2016–17 fiscal year, the Department began developing an Intranet site to provide staff with access to departmental policies and directives. It planned to roll out the site by the end of March 2017.
132. Security measures. Department officials informed us that they were taking steps to improve security measures. In particular, the Department had received approval to hire security guards for 10 health centres in the 2016–17 fiscal year.
133. Service delivery model. In June 2016, the Department awarded a contract to a consultant to complete the first phase of its service redesign project. The consultant was to consider the Department’s current service delivery model, examine delivery models in other selected jurisdictions, and propose options to redesign the delivery model.
About the Audit
The Office of the Auditor General’s responsibility was to conduct an independent examination of the Government of Nunavut’s management of selected health care personnel to provide objective information, advice, and assurance to assist the Legislative Assembly in its scrutiny of the government’s management of resources and programs.
All of the audit work in this report was conducted in accordance with the standards for assurance engagements set out by the Chartered Professional Accountants of Canada (CPA) in the CPA Canada Handbook—Assurance. While the Office adopts these standards as the minimum requirement for our audits, we also draw upon the standards and practices of other disciplines.
As part of our regular audit process, we obtained management’s confirmation that the findings reported in this report are factually based.
Objective
The audit objective was to determine whether the Department of Health, in coordination with the Department of Finance, had adequately managed its health care personnel to deliver services in local and regional health centres in Nunavut.
Scope and approach
The audit examined orientation and training, quality assurance processes, the management of safety risks facing staff working in health centres, and the recruitment of health care personnel. The audit also examined the planning and resourcing of health centres.
The audit team interviewed senior managers, health care providers (such as supervisors of health programs, community health nurses, physicians, X-ray takers, and clerk interpreters), as well as community representatives and representatives from Inuit organizations. We visited local and regional health centres in seven communities. The centres were of different sizes and were located in the three regions of Nunavut: Kitikmeot, Kivalliq, and Qikiqtaaluk. For the purposes of this audit, the term “community health centres” refers to local and regional centres, unless otherwise noted.
The audit involved reviewing and analyzing key documents and testing files pertaining to community health centres and health care personnel. We reviewed staffing actions for 72 clinical and non-clinical positions across the three regions. This included staffing actions related to supervisors of health programs (the nurses in charge of health centres), community health nurses, nurse practitioners, radiologists, ultrasonographers, clerk interpreters, and selected senior management positions.
We included the Department of Finance in the audit due to its role in the recruitment and staffing process.
We did not examine public health, mental health, long-term and community care, the management of contracts (such as those for physicians), financial and management controls over medical travel, the implementation of information technologies (telehealth and electronic health records), capital planning, or facilities management (such as health centres and boarding homes). We also did not audit the management of the Qikiqtani General Hospital in Iqaluit.
Criteria
To determine whether the Department of Health, in coordination with the Department of Finance, adequately managed its health care personnel to deliver services in local and regional health centres in Nunavut, we used the following criteria:
| Criteria | Sources |
|---|---|
|
The Department of Health defines the types and levels of services to be provided. |
|
|
The Department of Health provides Nunavummiut with the opportunity to participate in the development, design, and method of delivery of health services, and the Department of Health takes their input into account. |
|
|
The Department of Health has a human resource plan in place that reflects an allocation of resources based on the defined types and levels of services to be provided. |
|
|
The Department of Health, in coordination with the Department of Finance, manages recruitment in a way that meets the staffing needs of the Department of Health. |
|
|
The Department of Health provides orientation and training that enables health care personnel to acquire, maintain, and develop the skills and competencies they need to carry out their responsibilities. |
|
|
The Department of Health assures the quality of the services provided by health care personnel. |
|
|
The Department of Health provides a safe environment for health care personnel. |
|
Management reviewed and accepted the suitability of the criteria used in the audit.
Period covered by the audit
The audit covered the period between 1 April 2014 and 31 March 2016. Audit work for this report was completed on 10 January 2017.
Audit team
Assistant Auditor General: Jerome Berthelette
Principal: James McKenzie
Director: Liliane Cotnoir
Alexandre Boucher
Samira Drapeau
Merkevia Isaac
Élyse Maisonneuve
David Oommen
Adrienne Scott
Lisa Seguin
List of Recommendations
The following is a list of recommendations found in the report. The number in front of the recommendation indicates the paragraph where it appears in the report. The numbers in parentheses indicate the paragraphs where the topic is discussed.
Supporting health centre personnel
| Recommendation | Response |
|---|---|
|
39. The Department of Health should ensure that appropriate orientation and training are made available on a timely basis to its health care personnel. (19–38) |
The Department of Health’s response. Agreed. The Department of Health will formalize a plan to provide structured clinical orientation and training to health care personnel and will collaborate with the Department of Culture and Heritage on cultural orientation to ensure that it is provided in a timely manner to all new employees. |
|
41. The Department of Health should put in place systems to track and monitor whether its health care personnel have taken orientation and training in a timely manner and if licences and certifications are up to date. (40) |
The Department of Health’s response. Agreed. The Department of Health will formalize and implement a plan to track and monitor training, orientation, licensing, and certifications on an ongoing basis. |
|
55. The Department of Health should, in collaboration with the Department of Finance, develop and implement procedures for assessing and tracking the performance of casual and agency nurses. (42–54) |
The Department of Health’s response. Agreed. The Department of Health will engage in discussion with the Department of Finance on the amendment of the process to develop the necessary forms to accurately assess performance of casual health care staff and to secure a method to track and report on the performance of casual employees. The Department of Finance’s response. Agreed. The Department of Finance will work with the Department of Health to address performance reviews for casual and agency nurses, where appropriate, for the purpose of rehiring individuals. |
|
58. The Department of Health should ensure that its procedures for assuring and continuously improving the quality of its health care services are implemented according to departmental policy, including those related to monthly audits of patient charts and related annual reviews, annual community visits, performance appraisals, and incident reporting. It should also put systems in place to ensure that the findings resulting from these procedures are followed up on and implemented. (56–57) |
The Department of Health’s response. Agreed. The Department of Health will formalize a plan for the implementation of quality assurance that will include all aspects of the Office of the Auditor General of Canada’s recommendations. |
|
61. The Department of Health should ensure that its nursing manual is kept up to date and is well communicated to staff in health centres. (59–60) |
The Department of Health’s response. Agreed. The Department of Health will develop a schedule and procedure for the ongoing review and revision of the nursing manual. |
|
70. The Department of Health should systematically track and monitor safety-related incidents and take appropriate follow-up actions to correct or mitigate safety-related risks. (62–69) |
The Department of Health’s response. Agreed. The Department of Health will develop a health and safety strategy to include the tracking and statistical analysis of all health and safety-related incidents to ensure the proper actioning and allocation of resources to reduce risks. |
|
79. The Department of Health should, in collaboration with other departments, provide a safe and secure work environment for its health care personnel by implementing adequate procedures such as risk assessments and appropriate security measures. The Department should ensure that the security measures it implements are monitored, known, and working properly. (71–78) |
The Department of Health’s response. Agreed. The Department of Health will collaborate with the Department of Community and Government Services and the Department of Finance (Risk Management) to ensure that risks are identified and analyzed and that proper action is taken to address and reduce the potential for accident and injury. |
|
91. The Department of Health should develop procedures and service standards for its recruitment and staffing actions. The Department, with the collaboration of the Department of Finance and other relevant departments, should put systems and practices in place to track and record information related to vacancies and associated staffing actions, and look for opportunities to streamline the hiring process. (80–90) |
The Department of Health’s response. Agreed. The Department of Health will collaborate with the Department of Finance to improve information sharing and streamline the staffing process. The Department of Health will also develop standards and procedures to improve efficiency and expedite the hiring process. The Department of Finance’s response. Agreed. The Department of Finance will work on improving its internal information systems and on sharing this information with the Department of Health and other departments. |
|
92. The Department of Health and the Department of Finance should monitor the status of staffing actions and take appropriate action to reduce delays. This should include monitoring against their service standards. (80–90) |
The Department of Health’s response. Agreed. The Department of Health will collaborate with the Department of Finance to improve information sharing to reduce delays and monitor performance against service standards. The Department of Finance’s response. Agreed. The Department of Finance will collaborate with the Department of Health to improve information sharing to reduce delays and monitor performance against service standards. |
|
97. The Department of Finance and the Department of Health should work together to ensure that the terms and conditions of employment for health care positions are competitive, and should analyze the terms and conditions of employment in other provinces and territories when applicable. (93–96) |
The Department of Finance’s response. Agreed. The Department of Finance will collaborate with the Department of Health to develop market analysis and methodology for addressing any identified gaps in compensation for health care personnel to ensure that Nunavut is viewed by health care personnel as an employer of choice. The Department of Health’s response. Agreed. The Department of Health will seek assistance from the Department of Finance to develop market analysis and methodology for addressing gaps in compensation for health care personnel to ensure that Nunavut is viewed by health care personnel as an employer of choice. |
|
98. The Department of Health, in collaboration with the Department of Finance, should assess the market conditions for permanent, agency, and casual nurses; compare the results with other jurisdictions; and take appropriate actions based on this analysis to increase the competitiveness of these positions and facilitate the hiring of permanent nurses. (93–96) |
The Department of Health’s response. Agreed. The Department of Health will seek assistance from the Department of Finance to conduct a jurisdictional scan on compensation and non-monetary benefits across employment types to ensure that permanent employment is viewed as the most attractive employment option. The Department of Finance’s response. Agreed. The Department of Finance will collaborate with the Department of Health to conduct a jurisdictional scan on compensation and non-monetary benefits across employment types to ensure that permanent employment is viewed as the most attractive employment option. |
|
100. The Department of Health should complete the implementation of the recent initiatives to improve its human resource function, periodically assess the efficiency of these initiatives, and take appropriate actions on the results of these assessments. (99) |
The Department of Health’s response. Agreed. The Department of Health continues to work toward meeting deliverables outlined in the Department’s human resource strategy. Once completed, the strategy, which ends in 2017, will be evaluated and new actions will be included in the 2017–2020 strategy. |
|
103. The Department of Health should develop and implement an up-to-date nursing recruitment and retention strategy. (102) |
The Department of Health’s response. Agreed. The Department of Health has begun work on the new Health Professionals Recruitment and Retention Strategy, which includes nurses and other key health care staff. Non-monetary items will be implemented immediately, and monetary items will be prepared for discussion during the next contract negotiations, which will take place after the expiry of the current collective agreement in 2018. |
Planning and resourcing health centres
| Recommendation | Response |
|---|---|
|
118. The Department of Health should continue its efforts to review and improve how it delivers services to Nunavummiut. The Department should also put in place procedures that allow it to periodically assess how it delivers services to ensure that health centres are able to meet the demographic changes and needs of communities. (104–117) |
The Department of Health’s response. Agreed. The Department of Health is currently working on a new model. Once implemented, the model will be assessed and follow-up consultations will be held per article 32 of the Nunavut Land Claims Agreement. |
|
120. The Department of Health should develop and implement a human resource plan that ensures the Department has the right number and types of health care personnel needed to deliver health care services in Nunavut. (119) |
The Department of Health’s response. Agreed. A personnel mix strategy is included in the model of care project that is currently under way. This project is currently assessing health care centre needs and the personnel required to deliver those services and is expected to be completed by 31 March 2017. |
|
122. The Department of Health should implement systems and practices to collect and analyze key and meaningful information on the health of Nunavummiut and the services they receive at health centres in order to better inform its planning and decision making on providing health services. (121) |
The Department of Health’s response. Agreed. The model of care project will address data collection and analysis requirements identified in the audit. The project is expected to be completed by 31 March 2017. |
|
125. The Department of Health should ensure that Nunavummiut are involved throughout its current and future reviews of how it delivers health services and programs. (123–124) |
The Department of Health’s response. Agreed. The Department of Health will ensure that all strategy development requirements will continue to meet obligations under article 32 of the Nunavut Land Claims Agreement. |