Mental Health Services in Rural Yukon—Department of Health and Social Services—Infographic
Text version
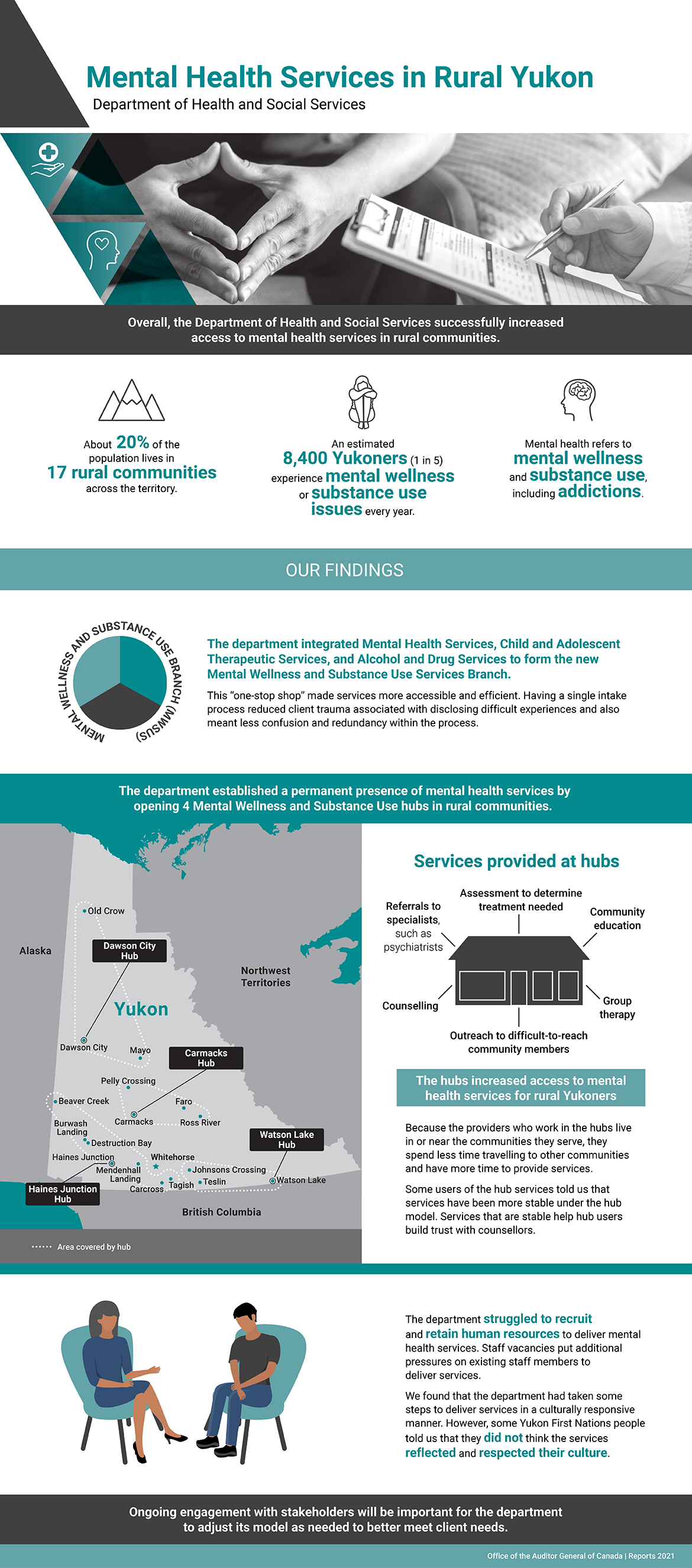
This infographic presents the findings from the audit on mental health services in rural Yukon.
The audit found that, overall, the Department of Health and Social Services successfully increased access to mental health services in rural communities.
Mental health in rural Yukon
About 20% of the population lives in 17 rural communities across the territory, and an estimated 8,400 Yukoners (1 in 5) experience mental wellness or substance use issues each year. In this audit, the term “mental health” refers to mental wellness and substance use, including addictions.
Our findings
Mental Wellness and Substance Use Services Branch
The department integrated Mental Health Services, Child and Adolescent Therapeutic Services, and Alcohol and Drug Services to form the new Mental Wellness and Substance Use Services Branch.
This “one-stop shop” made services more accessible and efficient. Having a single intake process reduced client trauma associated with disclosing difficult experiences and also meant less confusion and redundancy within the process.
Mental Wellness and Substance Use hubs
The department also established a permanent presence of mental health services by opening 4 Mental Wellness and Substance Use hubs to serve the following rural communities:
- In the north of the territory, the Dawson City Hub serves the communities of Dawson City, Mayo, and Old Crow.
- In the centre of the territory, the Carmacks Hub serves the communities of Carmacks, Faro, Pelly Crossing, and Ross River.
- In the southwest of the territory, the Haines Junction Hub serves the communities of Haines Junction, Beaver Creek, Burwash Landing, Carcross, Destruction Bay, Mendenhall Landing, and Tagish.
- In the south of the territory, the Watson Lake Hub serves the communities of Watson Lake, Johnsons Crossing, and Teslin.
These hubs increased access to mental health services for rural Yukoners by providing them with the following services:
- assessment to determine treatment needed
- community education
- group therapy
- outreach to difficult-to-reach community members
- counselling
- referrals to specialists, such as psychiatrists
Because the providers who work in the hubs live in or near the communities they serve, they spend less time travelling to other communities and have more time to provide services.
Some users of the hubs told us that services have been more stable under the hub model. Services that are stable help hub users build trust with counsellors.
Human resources
The department struggled to recruit and retain human resources to deliver mental health services. Staff vacancies put additional pressures on existing staff members to deliver services.
Cultural responsiveness
We found that the department had taken some steps to deliver services in a culturally responsive manner. However, some Yukon First Nations people told us that they did not think the services reflected and respected their culture.
Ongoing engagement with stakeholders will be important for the department to adjust its model as needed to better meet client needs.