2023 Report of the Auditor General of Canada to the Legislative Assembly of NunavutCOVID-19 Vaccines in Nunavut
Independent Auditor’s Report
Table of Contents
- Introduction
- Findings and Recommendations
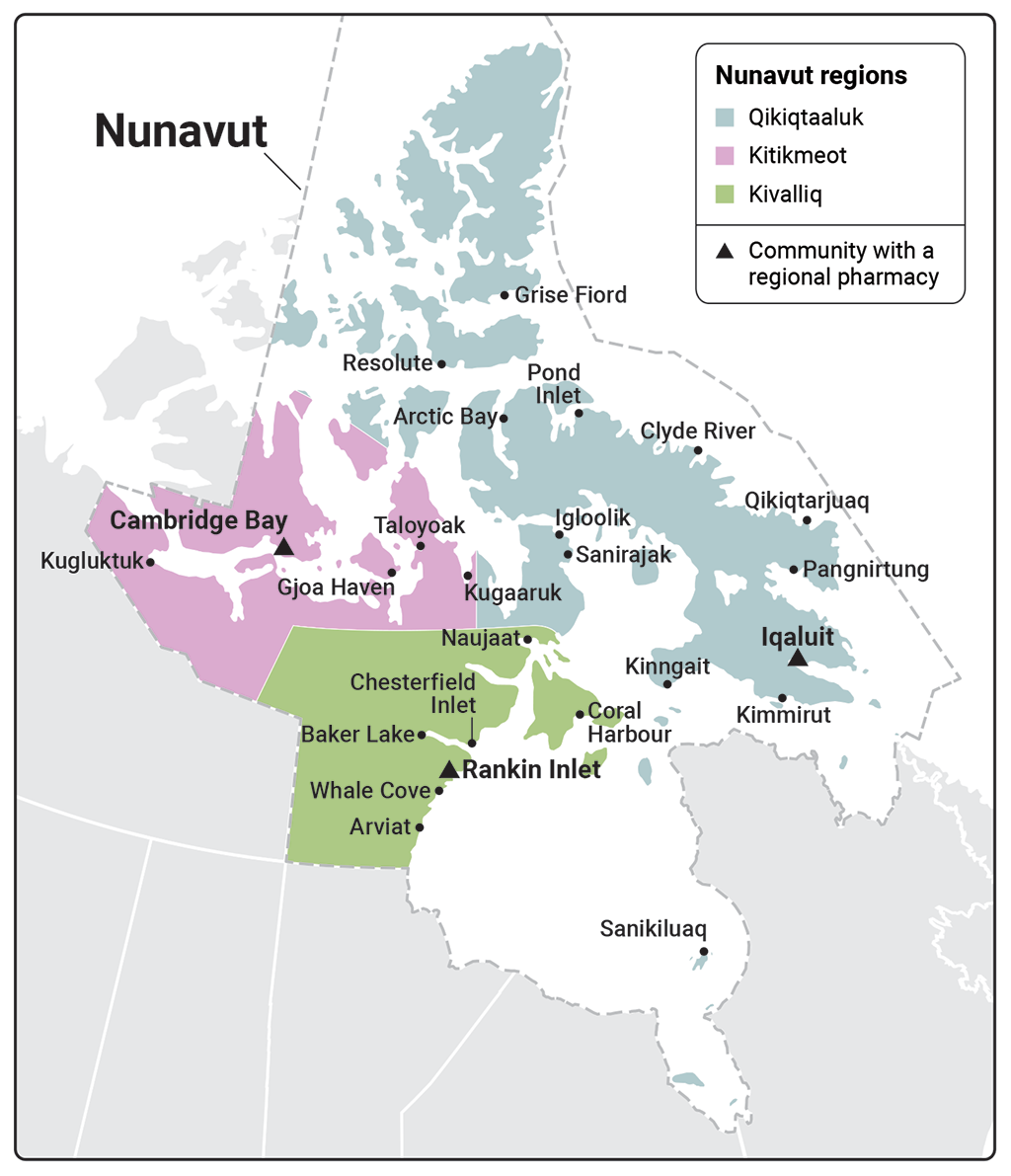
- Conclusion
- About the Audit
- Recommendations and Responses
- Exhibits:
- 1—Key dates in Nunavut’s COVID‑19 vaccine rollout
- 2—Nunavut’s 25 communities are dispersed across a vast area covering one fifth of Canada
- 3—Inuit societal values
- 4—COVID‑19 vaccine authorized and delivered to Nunavut
- 5—COVID‑19 vaccination coverage was lower in Nunavut than in Canada
- 6—Delivery route of COVID‑19 vaccine doses
- 7—As at September 2022, up to 31% of doses may have been wasted
Introduction
Background
1. The global outbreak of the coronavirus disease (COVID‑19)Definition 1 created a public health emergency that necessitated responses by international organizations and by the governments of Canada and Nunavut (Exhibit 1).
Exhibit 1—Key dates in Nunavut’s COVID‑19 vaccine rollout
| 25 January 2020 | The first case of COVID‑19 is confirmed in Canada. |
|---|---|
| 11 March 2020 | The World Health Organization declares the global outbreak of COVID‑19 to be a pandemic. |
| 20 March 2020 | The Government of Nunavut’s Minister of Health declares a state of public health emergency under section 40 of the Consolidation of Public Health Act. |
| 6 November 2020 | The first community case of COVID‑19 is confirmed in Nunavut. |
| 9 December 2020 | Health Canada authorizes the first COVID‑19 vaccine. |
| Mid‑December 2020 | Canada receives its first shipments of COVID‑19 vaccine doses. |
| 30 December 2020 | Nunavut receives its first shipments of COVID‑19 vaccine doses. |
| 6 January 2021 | Vaccination begins in Nunavut for people aged 18 years and older. |
| 15 June 2021 | Vaccination begins in Nunavut for people aged 12 years and older. |
| 30 November 2021 | Vaccination begins in Nunavut for people aged 5 years and older. |
| 11 April 2022 | Nunavut’s state of public health emergency officially ends. |
Source: The World Health Organization and various sources of the Government of Canada and the Government of Nunavut
2. Vaccines are considered to be one of the most important public health tools available for preventing serious illness and controlling infectious disease outbreaks. In December 2020, the federal, provincial, and territorial governments established Canada’s COVID‑19 Immunization Plan: Saving Lives and Livelihoods. Its goal was to enable immunization against COVID‑19 for as many Canadians as quickly as possible while ensuring the prioritization of high‑risk populations.
3. As part of the plan, the federal government procured and paid for the COVID‑19 vaccines, a certain amount of cold chain equipment (that is, freezers and thermal containers to maintain the requisite low temperatures), and related essential supplies, such as needles and syringes. During the COVID‑19 pandemic, the federal government also managed and covered the cost of vaccine delivery to the provinces and territories. The Government of Nunavut was responsible for allocating, delivering, and administering COVID‑19 vaccine doses within the territory and for monitoring and reporting on the rollout.

Apex, Nunavut
Photo: iStock.com/
Henry Baillie-Brown
4. The governments of Nunavut, Yukon, and the Northwest Territories requested that the federal government give them priority to receive the COVID‑19 vaccine that had the less stringent storage requirements. They did this because of the difficulties associated with delivering vaccines to remote and isolated northern communities. The federal government agreed to the request, and Nunavut received its first shipment of Moderna’s COVID‑19 vaccine doses on 30 December 2020.
5. Nunavut is the jurisdiction covering the largest area in Canada, nearly 1.9 million square kilometres. In the territory’s 3 regions of Qikiqtaaluk, Kivalliq, and Kitikmeot, the approximately 40,000 Nunavummiut are dispersed in 25 communities, which rely on air transportation (Exhibit 2).
Exhibit 2—Nunavut’s 25 communities are dispersed across a vast area covering one fifth of Canada
Source: Based on information from the Government of Nunavut’s Department of Health
Exhibit 2—text version
This map shows Nunavut’s 3 regions and 25 communities. One community in each region has a regional pharmacy.
Nunavut’s largest region is Qikiqtaaluk, which makes up the territory’s eastern half and its northernmost and southernmost areas. This region contains 13 of the territory’s 25 communities. In alphabetical order, they are Arctic Bay, Clyde River, Grise Fiord, Igloolik, Iqaluit, Kimmirut, Kinngait, Pangnirtung, Pond Inlet, Qikiqtarjuaq, Resolute, Sanikiluaq, and Sanirajak. The community with a regional pharmacy is Iqaluit.
The other 2 regions make up the territory’s western half. They are Kitikmeot to the north and Kivalliq to the south.
The region of Kitikmeot contains 5 of the territory’s communities. In alphabetical order, they are Cambridge Bay, Gjoa Haven, Kugaaruk, Kugluktuk, and Taloyoak. The community with a regional pharmacy is Cambridge Bay.
The region of Kivalliq contains the remaining 7 of the territory’s communities. In alphabetical order, they are Arviat, Baker Lake, Chesterfield Inlet, Coral Harbour, Naujaat, Rankin Inlet, and Whale Cove. The community with a regional pharmacy is Rankin Inlet.
6. Historical and socio-economic factors influence the health of Inuit Nunavummiut and their trust in government health care practices. Inuit make up approximately 85% of the population of Nunavut. According to data from the 2021 Census, Statistics Canada reported that more than half of Inuit in Nunavut live in overcrowded homes, where respiratory viruses can spread rapidly. All Nunavummiut also face barriers to accessing health care services because few facilities in the territory are able to offer specialized and intensive care. Nunavummiut needing such care often have to be transported by air to the hospital in Iqaluit or an out‑of‑territory health care facility. Most health care services in the territory are delivered by community nurses at community health centres.
7. Before the pandemic, there were chronic staffing shortages within the Department of Health. According to the Government of Nunavut’s Public Service Annual Report for the 2020–21 fiscal year, the Department of Health had an overall job vacancy rate of 45%. In summer 2021, the health centres in Grise Fiord and Resolute Bay had to close temporarily. In 5 other communities, while health care centres remained open, staffing shortages restricted them to providing only emergency services for an average of 2 weeks during that summer.
8. The Government of Nunavut’s Department of Health is responsible for the territory’s public health measures, including public health emergency preparedness and response. In the territory’s COVID‑19 vaccine rollout, the department was specifically responsible for
- receiving, storing, allocating, delivering, and administering vaccine doses
- informing the population about COVID‑19 vaccines and their availability
- monitoring and reporting on data related to the COVID‑19 vaccine rollout, such as inventory of doses, coverage, and adverse events
9. The Department of Health and the Chief Public Health Officer are responsible for developing and updating pandemic plans, which specify the responsibilities and actions to be taken before, during, and after a pandemic outbreak at the territorial, regional, and community levels of health services within Nunavut.

An inukshuk in Nunavut
Photo: iStock.com/RyersonClark
10. The Government of Nunavut’s Department of Community and Government Services is responsible for procurement and contracting on behalf of the government. For the COVID‑19 vaccine rollout, this included chartering aircraft to transport the vaccine doses and nurse immunizers, procuring equipment, and renting sites for vaccination clinics.
11. The Government of Nunavut’s Department of Executive and Intergovernmental Affairs is responsible for ensuring that the government’s communications are timely, accurate, clear, objective, and complete and that information about its policies, programs, services, and initiatives is available in the territory’s 4 official languages (Inuktitut, Inuinnaqtun, English, and French). In a territorial crisis, the department is responsible for leading and coordinating the government’s communications.
12. Inuit societal values give the government the foundation on which to create programs, policies, and services that are culturally relevant and meet the needs of Nunavummiut. The Consolidation of Public Health Act stipulates that the public health system in Nunavut shall be based on Inuit societal values and that the Minister of Health and the Chief Public Health Officer must ensure that Inuit societal values are incorporated throughout the public health system of Nunavut (Exhibit 3).
Exhibit 3—Inuit societal values
Section 6 of Nunavut’s Consolidation of Public Health Act requires that the following Inuit societal values be incorporated throughout the territory’s public health system:
| Inuit title | Meaning |
|---|---|
| Inuuqatigiitsiarniq | respecting others, relationships, and caring for people |
| Tunnganarniq | fostering good spirit by being open, welcoming, and inclusive |
| Pijitsirniq | serving and providing for family or community, or both |
| Aajiiqatigiinniq | decision making through discussion and consensus |
| Pilimmaksarniq or Pijariuqsarniq | the development of skills through practice, effort, and action |
| Piliriqatigiinniq or Ikajuqtigiinniq | working together for a common cause |
| Qanuqtuurniq | being innovative and resourceful |
| Avatittinnik Kamatsiarniq | respect and care for the land, animals, and the environment |
Focus of the audit
13. This audit focused on whether the Government of Nunavut’s Department of Health, Department of Executive and Intergovernmental Affairs, and Department of Community and Government Services managed the COVID‑19 vaccine rollout in an effective and equitable manner to protect the health and well‑being of Nunavummiut.
14. This audit is important because the COVID‑19 pandemic was the most severe outbreak of infectious disease in more than a century. Therefore, it is crucial to identify areas for improvement, capture lessons learned, and highlight successful strategies to support future public health emergency efforts, including support for health care workers. In addition, timely and equitable access to the COVID‑19 vaccines was important to lessen the negative impact of the virus on people and the health care system.
15. More details about the audit objective, scope, approach, and criteria are in About the Audit at the end of this report.
Findings and Recommendations
The responsible departments effectively and equitably delivered and administered vaccines
16. This finding matters because timely and equitable access to COVID‑19 vaccines was needed to help reduce the risk to Nunavummiut of serious illness, hospitalization, and death from COVID‑19. The provision of the COVID‑19 vaccines was an important public health priority to minimize the burden on Nunavut’s health care system.
17. The Moderna vaccine for people aged 18 years and older was selected for Nunavut because, unlike other vaccines, it did not require transportation in ultra‑cold temperatures. This vaccine was authorized by Health Canada on 23 December 2020. Nunavut received its first shipment of Moderna vaccine doses in late December 2020 (see Exhibit 4), and the territory’s vaccine rollout started in January 2021. The Public Health Agency of Canada allocated vaccine doses to each province and territory on a per‑capita basis, as agreed upon by the federal, provincial, and territorial governments in December 2020. Nunavut was one of the first of Canada’s territorial and provincial jurisdictions to receive COVID‑19 vaccines. As a result, the Government of Nunavut undertook the task of rolling out the vaccines to its population without having the benefit of lessons learned in other Canadian jurisdictions.
Exhibit 4—COVID‑19 vaccine authorized and delivered to Nunavut
| Vaccine manufacturer | Intended age range | Date authorized by Health Canada | Date received in the territory |
|---|---|---|---|
| Moderna | 18 years and older | 23 December 2020 | 30 December 2020 |
| Pfizer | 12 years and older | 5 May 2021 | 7 June 2021 |
| Pfizer | 5 years and older | 19 November 2021 | 27 November 2021 |
| Moderna | 6 months to under 6 years | 14 July 2022 | 20 July 2022 |
Source: Drug and Vaccine Authorizations for COVID‑19 website, Government of Canada
18. The Department of Health and the Department of Community and Government Services chartered flights to deliver vaccines and nurses to Nunavut communities. According to the Department of Health, it spent an incremental amount of $3.2 million on the COVID‑19 vaccine rollout, 78% (or more than $2.5 million) of which covered aircraft charter services.
Timely delivery to communities
19. We found that the Department of Health and the Department of Community and Government Services delivered COVID‑19 vaccine doses throughout the territory in a timely manner. We calculated that the departments delivered the vaccine doses and began immunizing people in communities in an average of 2 weeks after the vaccines arrived in the territory. In our view, deliveries were timely given the range of logistical challenges that the Department of Health faced in delivering the initial doses to the communities. The challenges included hiring and providing accommodation for nurse immunizers, securing transportation, adapting to weather conditions, and complying with the cold chain requirements for the vaccines.
Rapid administration of doses during mass vaccination clinics
20. At the beginning of the vaccine rollout in January 2021, the Department of Health organized mass vaccination clinics in each of the territory’s communities, except Iqaluit. It took this approach because of the logistics involved in flying vaccines and immunizers to communities and so that it could vaccinate eligible members of the population as quickly as possible. Once additional vaccines became available for younger age groups, community health centres offered other options to get vaccinated, including rolling schedules for vaccination appointments and having walk‑in clinics (that is, vaccination without making an appointment in advance). The mix varied in each location depending on the community’s needs.
21. Because of the limited Internet connectivity in rural and remote communities, there was no online booking system for the territory. People wanting to book an appointment for vaccination did so by phone or in person.
22. Iqaluit, Nunavut’s largest community, followed a staggered approach: Elders and members of the identified vulnerable groups were vaccinated first. Next, members of the general population became eligible for the vaccine on the basis of age group. The rollout in Iqaluit included mass vaccination clinics by appointment, followed by walk‑in clinics and regular appointments.
23. We found that to support the vaccine rollout, the Department of Health hired nurses from outside the territory on a temporary basis. Three teams of these nurses travelled by air from community to community in Nunavut to assist local community health care staff in administering the Moderna vaccine to people aged 18 years and older. During these first mass vaccination clinics in communities, the Department of Health succeeded in rapidly administering doses to the eligible population. The initial mass clinics operated for an average of 2.7 days in each community. We found that during the clinics, 45% of the eligible population received their first dose.
24. In June 2021, the Pfizer vaccine became available in Nunavut for people aged 12 years and older. To administer doses, the Department of Health continued to hire temporary nurses from out of territory and conducted mass vaccination clinics. The mass clinics operated for an average of 2 days in each community, including Iqaluit. We found that during the clinics, 39% of all 12- to 17‑year‑olds received their first dose.
25. We found that the Department of Health offered training on how to handle and administer vaccine doses before the immunizers performed this task in the communities. The department also provided immunizers with training on registration and documentation of vaccination. All immunizers were required to complete the Nunavut Immunization Certification. In addition, the department informed out‑of‑territory nurse immunizers that Inuit cultural training was available.
26. However, we found that the Department of Health did not track whether immunizers had completed the training available to them. In the Report of the Auditor General of Canada to the Legislative Assembly of Nunavut—2017, Health Care Services—Nunavut, we recommended that the Department of Health put in place systems to track and monitor whether its health care staff had taken orientation and training in a timely manner and whether licences and certifications were up to date. Although the department agreed with our recommendation in 2017, we found that it had not made progress on this issue.
27. As the Department of Health agreed to do in 2017, it should put in place systems to track the completion of orientation and training programs for health care staff, monitor whether their licences and certifications are up to date, and provide regular reports of overdue training and expired licences or certifications.
The department’s response. Agreed.
See Recommendations and Responses at the end of this report for detailed responses.
Priority given to vulnerable populations
28. To support equitable access to vaccination, the Department of Health identified vulnerable populations according to guidance from Canada’s National Advisory Committee on Immunization for the prioritization of initial doses. The department also took into account Nunavut’s context and its supply of vaccine doses. Those identified for prioritization included Elders, as well as individuals living in continuing care centres, correctional facilities, or shelters—and, by consequence, the populations of communities where these facilities were located. Moreover, the department prioritized communities experiencing an outbreak of COVID‑19 and communities at high risk of an outbreak. We found that the Department of Health gave guidance to its health care workers on prioritizing populations.
29. In Iqaluit, we found that the Department of Health prioritized identified vulnerable populations ahead of the general population and that communities prioritized by the department were vaccinated before other communities. On average, communities with facilities for vulnerable populations, such as continuing care centres, correctional facilities, or shelters, received the vaccine doses in half the number of days compared with communities without such facilities. We noted, however, that a community with a facility for an identified vulnerable population was omitted from the department’s prioritization, and thus this community received its first doses at the beginning of March 2021, after 9 communities without such facilities. This omission occurred because the Department of Health lacked information on vulnerable populations that would have helped support decision making in emergency situations.
Efforts to remove barriers to vaccination
30. We found that the Department of Health reduced vaccination barriers for vulnerable populations by bringing doses to them instead of expecting them to come to the vaccination sites. For example, to administer doses, the department’s community nursing staff travelled to local continuing care centres, to Elders’ homes, to correctional facilities, and to shelters. In Iqaluit, mobile units of nurses travelled by bus to vaccinate hard‑to‑reach populations.
31. We found that the Department of Health offered to vaccinate non‑residents who were temporarily in Nunavut. When the supply of doses was limited in the early months of the rollout, the department gave guidance to prioritize Nunavummiut and to offer vaccination to non‑residents only if additional doses were available in order to avoid wastage. In April 2021, non‑residents officially became eligible for vaccination.
32. In an effort to remove barriers to vaccination, the Department of Health arranged for Inuit community health representatives and interpreters to greet individuals arriving at vaccination clinics, offer translation services to them, explain consent forms, and provide vaccination fact sheets. In some communities, nurses contacted eligible community members to book appointments at a vaccination clinic.
Lower vaccination coverage because of large population under age 18
33. Of all of Canada’s provinces and territories, Nunavut had the lowest vaccination coverage. As at September 2022, coverage for 2 doses of COVID‑19 vaccine ranged from 73% to 78% in Nunavut’s 3 regions. The overall coverage for 2 doses in Nunavut (77%) was lower than the coverage for Canada (81%) (Exhibit 5).
Exhibit 5—COVID‑19 vaccination coverage was lower in Nunavut than in Canada
| Type of dose | Overall population coverage, January 2021 to September 2022 | |
|---|---|---|
| Nunavut | Canada | |
| Dose 1 | 83% | 84% |
| Dose 2 | 77% | 81% |
| Booster | 47% | 49% |
Source: Based on information from the Government of Nunavut’s Department of Health and the Public Health Agency of Canada
34. Nunavut had lower coverage than Canada overall because Nunavut’s population is significantly younger than that of Canada. People under the age of 18 make up about 37% of Nunavummiut. In contrast, the same age group makes up only 19% of the Canadian population. This is important because COVID‑19 vaccination coverage was lower for people under the age of 18 in Canada compared with adults aged 18 years and older. The coverage for people under the age of 18 was approximately 43% in Nunavut and 42% in Canada.
35. We calculated that if Canada had the same proportion of people under the age of 18 as Nunavut, the overall Canadian coverage would be lower than that of Nunavut. If we aligned the proportion of people under the age of 18 in Canada and in Nunavut, the Canadian coverage for the overall population that received 2 doses would decrease by 10 percentage points, making it 71% instead of 81%.
The departments collaborated on the vaccine rollout despite outdated plans
36. This finding matters because to limit the scope and public health impact of a pandemic, it is crucial to have a current and regularly updated pandemic plan with a clear governance structure, goals, and objectives. An important part of this plan is a comprehensive communications strategy, which provides reliable information on vaccination benefits and risks. Knowing these benefits and risks allows individuals to make sound decisions about how to protect their health.
37. This finding also matters because the COVID‑19 vaccine rollout required coordination by multiple departments within the Government of Nunavut. The Chief Public Health Officer and the Department of Health led the effort, but they had limited resources. The logistics for planning and implementing the rollout required a joint effort with other government departments, particularly the Department of Community and Government Services and the Department of Executive and Intergovernmental Affairs.
Gaps in pandemic plans and strategies
38. We reviewed whether the Government of Nunavut had plans and strategies in place to guide its efforts during the COVID‑19 vaccine rollout. We found that the Department of Health had influenza pandemic planning and response guidelines dating from 2012. Departmental officials informed us that the plans and response guidelines were not used because they were obsolete. The absence of a pandemic plan led to a lack of clarity about the roles and responsibilities of senior health officials during public health emergencies, as set out in the Consolidation of Public Health Act. Furthermore, there was a lack of guidance concerning how the department was to collaborate and consult with Inuit and community stakeholders.
39. Without a pandemic response plan, the Department of Health had to create and implement its vaccine rollout plans while the rollout was underway. However, the department informed us that it referred to guidance from Canada’s National Advisory Committee on Immunization on prioritizing initial doses and to the Public Health Agency of Canada’s guidance on planning immunization clinics and administering vaccine doses.
40. We found that the Department of Health and the Department of Executive and Intergovernmental Affairs developed a communications strategy for the COVID‑19 vaccine rollout. However, they did not update the strategy after March 2021. For this reason, they did not include communications activities specifically for the vaccination of people under 18 years of age.
41. In addition, we found that the communications strategy lacked not only performance indicators for measuring results against its objectives but also formal feedback mechanisms for assessing how communications activities were received. While we found that the 2 departments tracked the reach of their communications products, they did not assess the effectiveness of their efforts.
42. We found that the Consolidation of Public Health Act requires Inuit societal values to be incorporated into the territory’s public health system (see Exhibit 3). Representatives of the Department of Health told us that Inuit societal values were taken into account because they are incorporated and reflected in all activities of the Government of Nunavut. However, the department could not provide documentation on how it met this requirement in its COVID‑19 vaccine rollout planning.
43. The Department of Health should update its health emergency and pandemic plan to take into account changes to the Consolidation of Public Health Act and lessons learned from the COVID‑19 pandemic. The plan should
- clearly define roles and responsibilities
- specify how Inuit societal values will be taken into account
- include a communications strategy developed in collaboration with the Department of Executive and Intergovernmental Affairs, with formal performance indicators and feedback mechanisms
- include a documented process for engaging with Inuit and community stakeholders
The department’s response. Agreed.
See Recommendations and Responses at the end of this report for detailed responses.
Strong interdepartmental collaboration
44. We found that the Department of Health and the Department of Community and Government Services collaborated closely, especially at the start of the rollout, when they faced logistical challenges in delivering the vaccines. The 2 departments participated in the vaccine logistics working group created during the rollout. In this forum, they worked together to charter the flights that transported vaccine doses to communities. These flights also transported a mobile team of nurses who provided support to the health care workforce of community health centres by administering vaccine doses. The doses swiftly reached communities as a result of this collaboration (see paragraph 19).
45. We also found that the Department of Executive and Intergovernmental Affairs and the Department of Health collaborated closely. The 2 departments partnered to develop the COVID‑19 communications strategy. They were key members of the Central Communications Working Group, where they discussed COVID‑19–related communications activities and products. The strategy included sections on vaccination campaign communications and on ways to disseminate messages to target audiences.
46. We found that the Department of Health and the Department of Executive and Intergovernmental Affairs provided official communications for vaccination clinics in all 4 of Nunavut’s official languages (Inuktitut, Inuinnaqtun, English, and French). We selected a sample of 10 communities. We examined their communications for the first and second doses of the Moderna vaccine for people aged 18 years and older and their communications for doses of the Pfizer vaccine for people aged 12 years and older. Overall, we found that communications were clear and accurate about the date, time, and location of the clinics and about how to book an appointment to be vaccinated.
47. We found that to inform Nunavummiut throughout the territory about the COVID‑19 vaccines and vaccination clinics, the Department of Executive and Intergovernmental Affairs and the Department of Health used various modes of communication, including social media, radio, television, press conferences, and the Government of Nunavut’s official website. The 2 departments also kept track of public concerns expressed by participants in the 38 radio call‑in shows held by the Chief Public Health Officer. An interpreter was available for the call‑in shows during the Moderna vaccination campaign for people aged 18 years and older. The departments gathered and considered concerns expressed by Nunavummiut during press conferences and on relevant social media. With the input received, the departments were able to tailor subsequent events to take account of those concerns.
48. The Department of Health also relied on its Inuit community health representatives, local staff members of the department, to engage with the community in support of the vaccine rollout. These representatives provided COVID‑19 information on local radio programs, and they distributed the department’s communications materials to members of their communities.
Good collaboration with external stakeholders
49. We found that the 3 responsible departments engaged with Inuit and community stakeholders through working groups, where they received input about communications activities related to the vaccine rollout. We found that an interagency working group, made up of representatives of the Chief Public Health Officer, Government of Nunavut departments, the federal government, and Inuit organizations, met as needed and provided information on how best to coordinate efforts during the rollout. The responsible departments also held operational calls with municipal officials, where the departments offered help with the dissemination of messages related to COVID‑19 vaccination.
50. We found that the departments coordinated with an Inuit organization on planning and carrying out mass clinics where people aged 12 years and older received doses of the Pfizer vaccine. To supplement the mobile vaccination teams arranged by the Department of Health and to provide services in Inuktitut, an Inuit organization arranged for additional nurses, some of whom were Inuit, to join the vaccine rollout in Nunavut.
51. We found that the Department of Health encouraged community health centre staff to reach out to community stakeholders, such as municipal officials, to increase vaccination coverage. The department recognized the importance of seeking the help of community members in publicizing the vaccination clinics and reducing barriers to accessing vaccine doses. Community involvement took different forms. For example, municipalities and various community stakeholders offered free rides to vaccination clinics and promoted the clinics on radio.
The Department of Health had inadequate systems for monitoring and reporting data on the rollout
52. This finding matters because information such as vaccination coverage, inventory of doses on hand, and wastage of vaccine doses was crucial to help the Department of Health make well‑informed decisions on vaccine needs. It was also important to have adequate systems in place to monitor and report accurate and up‑to‑date information to Nunavummiut and the Government of Canada.
53. The Department of Health was able to order vaccine doses from the Public Health Agency of Canada. The initial quantities were determined on the basis of the federal agency’s allocation per capita, as agreed upon by the federal, provincial, and territorial governments. Later quantities were determined by the Government of Nunavut on the basis of needs. The federal government shipped doses mainly to 2 of the territory’s 3 regional pharmacies, located in Iqaluit and Rankin Inlet. Nunavut’s third regional pharmacy in Cambridge Bay later became an additional point of delivery. Regional pharmacies had the facilities required for storing COVID‑19 vaccines at the required temperatures until expiry. Each regional pharmacy supplied vaccine doses to the community health centres in the region it served (Exhibit 6). Most community health centres had cold storage facilities capable of storing COVID‑19 doses for only around 30 days.
Exhibit 6—Delivery route of COVID‑19 vaccine doses

Exhibit 6—text version
This illustration shows the delivery route of COVID‑19 vaccine doses in Nunavut. Doses are transported by air to Nunavut’s 3 regional pharmacies. The doses are then transported by air from the pharmacies to the community health centres in the regions that the pharmacies serve. Doses are administered to individuals at community health centres.
54. Until March 2022, the Department of Health and the Department of Executive and Intergovernmental Affairs posted weekly reports about COVID‑19 vaccination coverage on the Government of Nunavut’s website.
55. As it did with other jurisdictions in Canada, starting in January 2021, the Public Health Agency of Canada asked the Government of Nunavut to submit reports at least once a week on
- the number of vaccine doses administered by product
- vaccine recipients, with information such as their sex, age, race, ethnicity, Indigenous status, and key populations (for example, health care workers or individuals in congregate living)
- vaccine doses wasted
- adverse events linked to vaccinations, with details about serious adverse events
COVID‑19 vaccine data reporting timely but not consistently accurate
56. We found that the Department of Health reported in a timely manner to the Public Health Agency of Canada on vaccination coverage and inventory wastage and on the vaccination coverage of several vulnerable populations. We analyzed a selected sample of reports and observed that they were submitted weekly as requested by the agency.
57. The Department of Health gathered data and reported it to the Public Health Agency of Canada by product, dose, sex, and age of the recipient, as requested. In addition, the agency asked provinces and territories to report coverage of adults in remote and isolated Indigenous and northern communities. Because the entire adult population of Nunavut fell into this category, the territory did not disaggregate the data to report more specifically on Inuit Nunavummiut.
58. We also found that the Department of Health did not monitor the COVID‑19 vaccination coverage of Inuit Nunavummiut even though it was able to identify individuals with Inuit status who had been vaccinated. We therefore analyzed Nunavut’s COVID‑19 vaccination records collected by the Department of Health, and we were able to ascertain that 75% of the Inuit population had received 2 vaccine doses. By not disaggregating the data to identify Inuit Nunavummiut, the Department of Health may have missed opportunities to tailor its public health strategies.
59. Departmental health care staff used paper-based forms to document adverse events following immunization, defined by the Public Health Agency of Canada as any untoward occurrence that follows immunization and is not necessarily caused by it. These forms were to be reviewed by departmental officials and then submitted to the Public Health Agency of Canada. We noted inconsistencies and discrepancies in the spreadsheets used by the Department of Health to track and report adverse events. We also noted the omission of information on the severity of the events. We found that from 1 January 2021 to 31 October 2022, as a result of an ineffective system for managing adverse events, the department had recorded a total of 95 adverse events following immunization, but the Public Health Agency of Canada had received only 87 adverse event reports. Without an efficient tracking and reporting system, there was a risk that the department might not report adverse events in an appropriate and timely manner to the Public Health Agency of Canada. The use of a manual system also increased the risk of errors.
60. To prepare for future public health emergencies, the Department of Health should implement a digital system enabling it to track and report on adverse events and disaggregated data in a complete, consistent, systematic, and timely manner.
The department’s response. Agreed.
See Recommendations and Responses at the end of this report for detailed responses.
Lack of inventory management system for tracking vaccine doses
61. As at September 2022, the Department of Health did not have a complete and accurate account of the COVID‑19 vaccine doses that it had received from the Public Health Agency of Canada. The department placed orders through VaccineConnect, the federal agency’s information technology solution released in 2021 for managing nationwide vaccination programs. However, as we noted in the 2022 Reports of the Auditor General of Canada to the Parliament of Canada, Report 9—COVID‑19 Vaccines, VaccineConnect was not fully operational at the start of the vaccine rollout. Although the Department of Health could not generate a report of all the vaccine doses that it had ordered and received from the federal government through VaccineConnect, this information was available from the Public Health Agency of Canada on request.
62. We found that the Department of Health did not have a complete and consistent method of tracking the movement of vaccine doses from the regional pharmacies to community health centres. We noted information errors and inconsistencies in the various spreadsheets used to track inventory and omissions of key information, such as lot numbers and expiry dates. Regional pharmacies maintained manual records of their vaccine inventory, but the department did not track how many doses were available at community health centres and therefore did not have a complete picture of the inventory of doses. Complete and accurate inventory information—including supplies of vaccine doses, lot numbers, and expiry dates—is important to support safe and cost‑effective health care.
63. We found that the Department of Health used a time‑consuming manual system for tracking wastage of doses. In addition, we found that the department did not have an effective system in place to distinguish between open‑vial and closed‑vial wastage. Because the tracking system increased the burden placed on health care staff, the department stopped tracking wastage at community health centres as of May 2022, with advanced approval from the Public Health Agency of Canada. However, at the regional pharmacies, the Department of Health continued to report wastage of closed vials that had expired. Having an effective inventory management system is important to facilitate the identification and use of doses that are close to their expiry date. This, in turn, would help avoid over‑ordering vaccine doses and would minimize wastage.
64. We found that the department reported a wastage of 18,151 doses (or 15%) as at September 2022. Because the tracking of wastage at the community health centres stopped in May 2022, the actual wastage rates were likely higher than the reported 15%. The sources of wastage included
- doses expired
- opened vials containing doses not administered
- vials not kept at the required temperatures
- storage and handling incidents
65. We found that because of poor record keeping and the lack of inventory tracking, the Department of Health could not account for 19,542 COVID‑19 vaccine doses (or 16%) as at September 2022. This figure represented the difference between the number of doses that the Public Health Agency of Canada had distributed to Nunavut and the sum of doses administered, doses on hand in inventory at the regional pharmacies, and doses known to be expired or wasted.
66. As we noted above, the Department of Health reported a wastage of 15% of doses received. However, since the department did not have systems to track inventory at the community health centres or to track wastage after May 2022, it did not know how many of the 19,542 doses that were unaccounted for (or 16%) were wasted or held in inventory. Therefore, with the inclusion of the doses that were unaccounted for, the department may have wasted more than double the amount of the doses reported (up to 31%) as at September 2022 (Exhibit 7). Some wastage was to be expected with the logistics to service remote communities with vaccines that required temperature control, the evolving nature of the COVID‑19 virus, changes in vaccine administration guidelines, and the decrease in vaccination demand as the pandemic progressed. However, wastage could have been minimized by having an effective tracking system to manage inventory and support an accurate needs assessment.
Exhibit 7—As at September 2022, up to 31% of doses may have been wasted
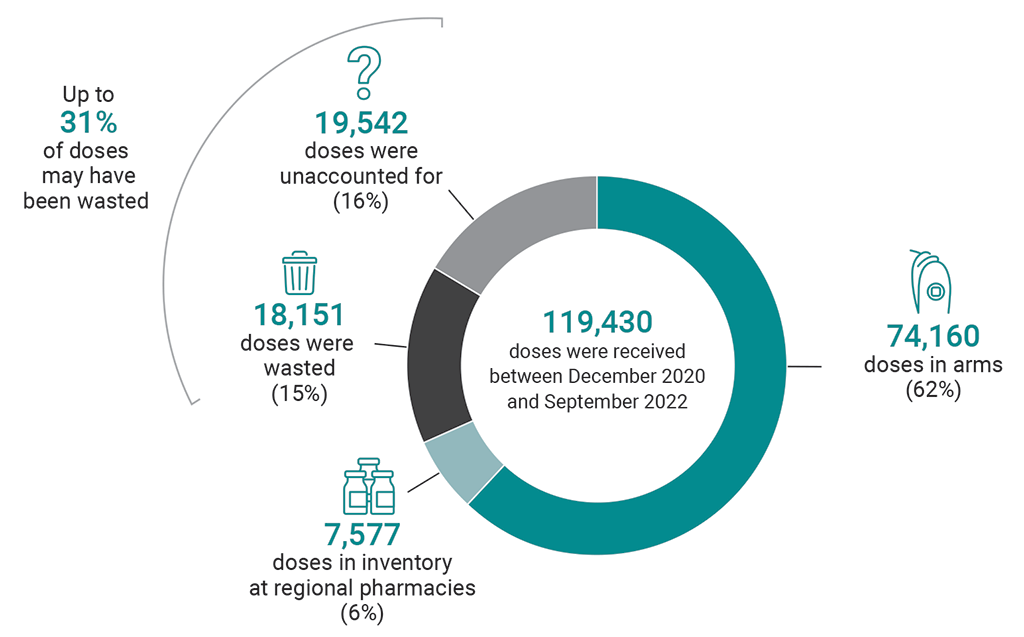
Note: Because of rounding, percentages do not total 100.
Source: Based on information from the Public Health Agency of Canada and the Government of Nunavut’s Department of Health
Exhibit 7—text version
This pie chart shows the breakdown of the 119,430 vaccine doses that Nunavut received between December 2020 and September 2022.
Up to 31% of the doses that were received may have been wasted. This consisted of the following:
- 19,542 doses that were unaccounted for, which represented 16% of the doses that were received
- 18,151 doses that were wasted, which represented 15% of the doses that were received
The remaining number of doses that were received consisted of the following:
- 74,160 doses in arms, which represented 62% of the doses that were received
- 7,577 doses in inventory at regional pharmacies, which represented 6% of the doses that were received
Note: Because of rounding, percentages do not total 100.
67. To improve inventory management at the territorial, regional, and community levels and to lighten the burden on its health care workers, the Department of Health should implement a digital inventory system capable of tracking medications, including vaccines and related medical supplies, from their entry into the territory to their administration or use. This should include the ability to track the movement of medications within the territory, lot numbers, expiry dates, usage, and wastage.
The department’s response. Agreed.
See Recommendations and Responses at the end of this report for detailed responses.
Conclusion
68. We concluded that the Government of Nunavut’s Department of Health, Department of Executive and Intergovernmental Affairs, and Department of Community and Government Services managed the COVID‑19 vaccine rollout in an effective and equitable manner to protect the health and well‑being of Nunavummiut. The Department of Health and the Department of Community and Government Services delivered vaccine doses to the remote communities of Nunavut in a timely manner, and the Department of Health was able to administer the doses rapidly. These successes were the results of effective interdepartmental collaboration and stakeholder engagement.
69. However, the Department of Health lacked the information systems to track, monitor, and report on key components of the vaccine rollout, such as vaccine inventory, wastage, adverse events, and training. As a result, the department may have wasted up to 31% of the doses received. In addition, the department did not have a pandemic plan in place to guide its COVID‑19 vaccination efforts.
About the Audit
This independent assurance report was prepared by the Office of the Auditor General of Canada on the COVID‑19 vaccine rollout in Nunavut. Our responsibility was to provide objective information, advice, and assurance to assist the Legislative Assembly of Nunavut in its scrutiny of the government’s management of resources and programs, and to conclude on whether the management of the COVID‑19 vaccine rollout in Nunavut complied in all significant respects with the applicable criteria.
All work in this audit was performed to a reasonable level of assurance in accordance with the Canadian Standard on Assurance Engagements (CSAE) 3001—Direct Engagements, set out by the Chartered Professional Accountants of Canada (CPA Canada) in the CPA Canada Handbook—Assurance.
The Office of the Auditor General of Canada applies the Canadian Standard on Quality Management 1—Quality Management for Firms That Perform Audits or Reviews of Financial Statements, or Other Assurance or Related Services Engagements. This standard requires our office to design, implement, and operate a system of quality management, including policies or procedures regarding compliance with ethical requirements, professional standards, and applicable legal and regulatory requirements.
In conducting the audit work, we complied with the independence and other ethical requirements of the relevant rules of professional conduct applicable to the practice of public accounting in Canada, which are founded on fundamental principles of integrity, objectivity, professional competence and due care, confidentiality, and professional behaviour.
In accordance with our regular audit process, we obtained the following from entity management:
- confirmation of management’s responsibility for the subject under audit
- acknowledgement of the suitability of the criteria used in the audit
- confirmation that all known information that has been requested, or that could affect the findings or audit conclusion, has been provided
- confirmation that the audit report is factually accurate
Audit objective
The objective of this audit was to determine whether the Department of Health, the Department of Executive and Intergovernmental Affairs, and the Department of Community and Government Services of Nunavut managed the COVID‑19 vaccine rollout in an effective and equitable manner to protect the health and well‑being of Nunavummiut.
Scope and approach
The audit scope included the Government of Nunavut’s Department of Health, Department of Executive and Intergovernmental Affairs, and Department of Community and Government Services. We examined how these departments managed the COVID‑19 vaccine rollout by developing plans, implementing and communicating them, and monitoring and reporting on core elements of the COVID‑19 vaccine rollout.
We examined the relevant legislation, plans, policies, and procedures related to the vaccine rollout in Nunavut. We interviewed officials from the audited departments and members of Inuit and community stakeholders. We conducted interviews with nurses, school principals, and staff of facilities that were prioritized for vaccination in all 3 regions of Nunavut. We also analyzed data on coverage rates, inventory, waste management, and adverse events.
We did not examine the following:
- the procurement of COVID‑19 vaccines
- the authorization of COVID‑19 vaccines
- the safety and effectiveness of the vaccines
- the appropriateness of the Department of Health’s sequencing and prioritization of populations eligible to receive doses
- the quality of training provided to immunizers
- the scientific accuracy of communications material on vaccines
- the psychological and physical impacts of the implementation of the vaccine rollout on health care workers in the territory
The rollout for children aged 6 months and older started in late July 2022. The most recent COVID‑19 immunization data that we received for this audit dated from mid‑September 2022. From late July to mid‑September, not enough data had been collected by the Department of Health to provide a representative picture of the coverage for this age group. Therefore, we excluded this age group from the scope of the audit.
Criteria
We used the following criteria to conclude against our audit objective:
| Criteria | Sources |
|---|---|
|
The Department of Health and the Department of Executive and Intergovernmental Affairs
The Department of Health and the Department of Executive and Intergovernmental Affairs
|
|
|
The Department of Health, the Department of Executive and Intergovernmental Affairs, and the Department of Community and Government Services
The Department of Health, the Department of Community and Government Services, and the Department of Executive and Intergovernmental Affairs
|
|
|
The Department of Health and the Department of Executive and Intergovernmental Affairs
The Department of Health and the Department of Executive and Intergovernmental Affairs
|
|
|
The Department of Health and the Department of Executive and Intergovernmental Affairs
The Department of Health and the Department of Executive and Intergovernmental Affairs
|
|
Period covered by the audit
The audit covered the period from 1 March 2020 to 31 October 2022. This is the period to which the audit conclusion applies.
Date of the report
We obtained sufficient and appropriate audit evidence on which to base our conclusion on 19 April 2023, in Ottawa, Canada.
Audit team
This audit was completed by a multidisciplinary team from across the Office of the Auditor General of Canada led by Markirit Armutlu, Principal. The principal has overall responsibility for audit quality, including conducting the audit in accordance with professional standards, applicable legal and regulatory requirements, and the office’s policies and system of quality management.
Recommendations and Responses
In the following table, the paragraph number preceding the recommendation indicates the location of the recommendation in the report.
| Recommendation | Response |
|---|---|
|
27. As the Department of Health agreed to do in 2017, it should put in place systems to track the completion of orientation and training programs for health care staff, monitor whether their licences and certifications are up to date, and provide regular reports of overdue training and expired licences or certifications. |
The department’s response. Agreed. The Department of Health will work with the other Government of Nunavut departments on the design of the human resource modules within the newly procured Enterprise Resource Planning system. Module deployment is scheduled for fall 2024. The system will track the completion of orientation and training programs for health care staff, monitor whether their licences and certifications are up to date, and provide regular reports of overdue training and expired licences or certifications. |
|
43. The Department of Health should update its health emergency and pandemic plan to take into account changes to the Consolidation of Public Health Act and lessons learned from the COVID‑19 pandemic. The plan should
|
The department’s response. Agreed. The Department of Health’s Office of the Chief Public Health Officer commits to learning lessons from the COVID‑19 pandemic and updating the department’s pandemic plan, with specific reference to recent changes to the Consolidation of Public Health Act, clearly defined roles and responsibilities, the incorporation of Inuit societal values, a communications strategy with integral performance indicators and feedback mechanisms, and a documented process for stakeholder and community engagement. Work is currently under way and should be completed by the end of 2023. The Department of Health’s Communications Division commits to working with the Department of Executive and Intergovernmental Affairs, the Office of the Chief Public Health Officer, and Department of Health leadership to build a communications strategy that can be incorporated into the pandemic plan. The plan will include tactics to ensure Inuit societal values are a foundational part of the plan, measurement tools to evaluate performance and gather public feedback, and processes to engage with Inuit and community stakeholders, including a documentation process for engagement activities. The Communications Division aims to complete this section of the plan by September 2023. |
|
60. To prepare for future public health emergencies, the Department of Health should implement a digital system enabling it to track and report on adverse events and disaggregated data in a complete, consistent, systematic, and timely manner. |
The department’s response. Agreed. The Department of Health commits to commence a planning project for Nunavut’s Public Health Surveillance System in 2023/24. The planning, facilitated by a consultant team, will achieve:
The Public Health Agency of Canada will be engaged during our planning phase and beyond to ensure alignment on required standards for integration. |
|
67. To improve inventory management at the territorial, regional, and community levels and to lighten the burden on its health care workers, the Department of Health should implement a digital inventory system capable of tracking medications, including vaccines and related medical supplies, from their entry into the territory to their administration or use. This should include the ability to track the movement of medications within the territory, lot numbers, expiry dates, usage, and wastage. |
The department’s response. Agreed. To improve inventory management at the territorial, regional, and community levels and to lighten the burden on our health care workers, the Department of Health commits to submitting a business case in summer 2023, requesting resources needed to advance a digital tracking system. The procurement process for a digital inventory management system would commence within 2 months of receiving project resources. The digital inventory tracking system will be able to track vaccines and other medications from entry into the territory to their administration. This should include the ability to track the movement of vaccines and medications within the territory, lot numbers, expiry dates, usage and wastage. As an interim measure, the Department of Health will create a manual tracking system by September 2023. |